Volume 10, Number 2—February 2004
THEME ISSUE
2004 SARS Edition
Preparedness and Response
Health Communication during SARS
Abstract
During the severe acute respiratory syndrome (SARS) outbreak, electronic media made it possible to disseminate prevention messages rapidly. The Centers for Disease Control and Prevention’s Travelers’ Health Web site was frequently visited in the first half of 2003; more than 2.6 million visits were made to travel alerts, advisories, and other SARS-related documents.
Experience with the outbreak of severe acute respiratory syndrome (SARS) has reinforced the importance of a multipronged approach to preventing disease transmission. Timely health communication, along with surveillance, quarantine, isolation, and travel restrictions, figured prominently among the tools the Centers for Disease Control and Prevention (CDC) used to help contain the outbreak. During the SARS response, health communication was shown to be an integral element by ensuring that knowledge about prevention measures reached the public, healthcare providers, the media, and other stakeholders.
Disseminating information and educational materials is a key element of CDC’s response to disease outbreaks that affect international travelers. Electronic media greatly expedite the process of dissemination and enable prevention messages to reach an expanded audience. The SARS response may be compared with a situation approximately 10 years before, when an outbreak of plague occurred in India (1). In both situations, the challenge was to control a disease outbreak that had potential for rapid international spread and to provide guidance tailored for specific audiences.
In late August 1994, CDC received reports from India of an epidemic of plague, the first such outbreak in 24 years. Within 2 months, 5,150 cases of either bubonic or pneumonic plague were reported to the World Health Organization from eight Indian states (2). Fifty-six deaths were reported, and >100,000 people fled Surat, a city of approximately 2 million. Neighboring nations closed their borders to travelers and cargo from India, and flights were discontinued.
CDC recognized the need for rapid dissemination of comprehensive educational materials to ameliorate the panic. By the end of September 1994, CDC had produced six documents to distribute to public health officials: an outbreak notice; a plague advisory for travelers to India; a plague alert notice handed to passengers arriving from India, which described the symptoms of plague and urged them to seek medical attention if they developed a febrile illness within 7 days; recommendations for treatment and prophylaxis; guidelines for diagnosis and biosafety; and a review article in the Morbidity and Mortality Weekly Report. These documents were disseminated through an automated fax information service, a voice information service, and a telephone hotline, as well as traditional print media. The fax service reported that 5,589 documents were requested regarding the plague outbreak.
Because of the high volume of air travel from India (approximately 2,000 arriving passengers daily at John F. Kennedy International Airport on flights from India), the departments of health in New York City and New York State supplemented CDC’s surveillance plan by using two approaches to disseminate information to heighten awareness of plague, focusing on emergency department physicians. First, a fact sheet was transmitted by fax or electronic mail to emergency department physicians and infection-control practitioners at 102 hospitals in New York City and to all acute-care hospitals and county health departments in the state. Second, a special plague advisory was distributed to 20,000 physicians in New York City (3).
The need for educational materials to heighten the awareness of healthcare providers and the public about SARS became obvious early in the outbreak. Because information was rapidly evolving, guidelines needed to be flexible. The “interim” document, one that required constant updating, became the norm. The Internet became a primary tool for communication, as it has been for CDC travelers’ health information. In fact, before the SARS outbreak, the travelers’ health Web site (located within the CDC Web site; available from: URL: www.cdc.gov\travel) had become the most frequently visited CDC Web site other than the home pages, with more than 3.6 million visits recorded in 2002 (Figure 1). Visits to the Web site increased dramatically in 2003. As of July, >4 million visits had been recorded to the travelers’ health Web site; more than 1 million of these visits resulted from accessing SARS-related content (travel alerts and advisories). Although the target audience for this Web site is in the United States, approximately one third of the visits were from other countries. In May, the city from which the most visits originated was Taipei, Taiwan, with more visits than any city in the United States. The SARS-related documents were not posted in multiple areas on the Web site but could be accessed by navigating through the Web site using different routes. Data from Web-tracking software showed that approximately 83% of visitors came from a commercial or .net domain, 10% from educational domains, 3% from .org domains, 2% from government domains, and 1.5% from military domains.
As part of the SARS response, CDC’s Division of Global Migration and Quarantine (DGMQ) developed travel-related information and recommendations, as well as industry-specific guidelines. Web sites that referred to these pages with a substantial number of visits included those from 1) organizations serving constituent groups such as families adopting children from Asia and expatriates overseas, 2) organizations with major meetings or conferences in areas with SARS, and 3) major news organizations. Overall, during the outbreak, DGMQ generated >125 documents, including updates and translations into seven languages, which were posted on the SARS pages of the CDC Web site. This material was written for multiple audiences, from highly technical to low literacy, and was disseminated through multiple platforms, from traditional print (e.g., >2,700,000 yellow Health Alert Notices were handed out by Quarantine Officers to passengers disembarking from 11,840 flights from areas with SARS) to electronic (postings on Web sites and CDC’s Secure Data Network).
As the outbreak matured and additional stakeholders were identified, interim guidelines were tailored to the specific concerns of healthcare providers, industry, and the traveling public (Table). Fact sheets explaining the legal authority for isolation and quarantine were written and posted. More than 1.5 million visits were made to DGMQ documents on CDC’s SARS Web site, in addition to the 4 million visits to the Travelers’ Health Web site.
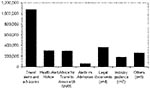
The travel alerts and advisories received the most visits (Figure 2). Historically, CDC has never advised against travel to any region, even during the plague epidemic in India. However, because of the rapid spread of SARS, its short incubation period, and the potential severity of illness, the need was recognized to codify different levels of concern about potential transmission to travelers. Thus, the travel alert and advisory system was developed.1
A travel alert is a notification by CDC that an outbreak of a disease is occurring in a geographic area. Its purpose is to provide information to travelers and resident expatriates about the status of an outbreak, how to reduce their risk for infection, and what to do if they become ill. The risk for individual travelers is thought to be definable and limited. In contrast, a travel advisory recommends against nonessential travel to an area because the risk to travelers is considered to be high as a result of ongoing transmission or inadequate containment. The travel advisory not only provides information about the status of an outbreak, but also is intended to reduce risk for exposure by decreasing the volume of traffic to the affected area.
These designations were used for the first time during the SARS outbreak, and thus criteria for their introduction, downgrading, and removal were required. Institution of either an alert or advisory was dependent on the magnitude and scope of the outbreak, the containment measures being used, the quality of surveillance in the affected area, and the quality and accessibility of medical care, all of which are based on reports from the involved countries. Once instituted, downgrading an advisory to an alert required adequate surveillance and no evidence of ongoing transmission for at least two incubation periods after the date of onset of symptoms in the last case (for SARS, 20 days). Removing an alert was dependent on the above criteria, as well as lack of evidence of new cases for three incubation periods (for SARS, 30 days) and no exportation of cases, as determined by an assessment of the information reported from the countries involved.2
During the outbreak, the relationship between DGMQ and the airline industry through the Airline Transport Association (ATA) and the airline medical directors was strengthened. As international spread of SARS through airline travel became a possibility, ATA was not only eager to provide information necessary for tracking passengers, but also served as a sounding board for specific guidelines for the traveler, flight crew, cargo handlers, and cleaning crew, and for the management of ill passengers. Other stakeholders included the cruise ship industry and U.S. citizens living overseas.
A comparison of the efforts in mass communication during the Indian plague outbreak that occurred in 1994 with those during SARS is illustrative of the changes that have resulted from the large increase in numbers of travelers, the decreased time in transiting the globe, and the massive demand for instant information (4). Electronic communications media enabled information to reach much wider audiences than had been possible through means such as traditional print media and fax services and allowed distribution of guidelines directed at specific target audiences. During the 1994 plague outbreak, thousands of documents were distributed by traditional means; during the SARS response, which lasted approximately the same time, millions of documents were disseminated through the CDC Web site.
Dr. Paul Arguin is team leader for zoonotic diseases in the Geographic Medicine and Health Promotion Branch of the Division of Global Migration and Quarantine, National Center for Infectious Diseases at Centers of Disease Control and Prevention. His research focuses on preventing zoonosis and imported infectious diseases.
References
- Fritz C, Dennis DT, Tipple M, Campbell GL, McCance CR, Gubler DJ. Surveillance for pneumonic plague in the United States during an international emergency: a model for control of imported emerging diseases. Emerg Infect Dis. 1996;2:30–6. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. International notes update: human plague–India, 1994. MMWR Morb Mortal Wkly Rep. 1994;43:761–2.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. Emerging infectious diseases detection of notifiable diseases through surveillance for imported plague–New York, September 1994. MMWR Morb Mortal Wkly Rep. 1994;43:805–7.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. International notes: human plague–India, 1994. MMWR Morb Mortal Wkly Rep. 1994;43:689–91.PubMedGoogle Scholar
Figures
Table
Cite This Article1In the 1994 plague documents, the term “advisory” did not have the same connotation.
2These criteria differed from those used by the World Health Organization.
Table of Contents – Volume 10, Number 2—February 2004
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Paul M. Arguin, Centers for Disease Control and Prevention, 1600 Clifton Rd., Mailstop E03, Atlanta, GA 30333, USA; fax: (404)498-1633
Top