Volume 10, Number 3—March 2004
Dispatch
Neisseria meningitidis C:2b:P1.2,5 with Intermediate Resistance to Penicillin, Portugal
Abstract
For 1 year, serogroup, serotype, serosubtype, and penicillin susceptibility of meningococci circulating in various regions in Portugal were evaluated. Most frequent phenotypes were B:4:P1.15 (13.4%) and C:2b:P1.2,5 (75.9%), which are also common in Spain. Overall, 27.5% of C:2b:P1.2,5 strains showed intermediate resistance to penicillin. Laboratory-based surveillance of meningococcal infection in Portugal provides important information to assess the adequacy of public health measures.
In Europe, infections caused by Neisseria meningitidis are associated with high rates of disease and death (1). Outbreaks of invasive meningococcal disease, including some cases of sudden death in some countries, suggest that vaccination may be necessary to reduce the incidence of this infection (2). Knowledge of the antigenic characteristics of N. meningitidis would help determine the most appropriate control strategies, which may vary from country to country.
Serogroups B and C are the most widespread, representing approximately 95% of cases of invasive meningococcal disease in Europe (1), and serogroup B is the most frequent cause of invasive meningococcal disease both in America and Europe (3). Serotypes and serosubtypes can be distinguished according to antigenic variants of the outer membrane proteins PorB and PorA (4).
In Portugal, the Compulsory Notifiable Diseases system is used, and meningococcal disease is a notifiable disease (5). The serogroup C conjugate vaccine was licensed in 2000, and vaccination has been voluntary since the third quarter of 2001. Laboratory analysis of serotypes and serosubtypes, not previously studied in meningococcal isolates from Portugal, would contribute to understanding meningococcal diversity and spread of meningococcal disease before the voluntary vaccination period.
We report a laboratory-based surveillance study of the N. meningitidis serogroups, serotypes, and serosubtypes in circulation in Portugal, as isolated from patients with cases of cultured-confirmed invasive infection. Susceptibility to penicillin was also evaluated.
A total of 116 isolates of N. meningitidis were detected through a laboratory surveillance study; 27 hospitals from different regions of Portugal participated. The investigation was conducted for 12 consecutive months (September 2000 to August 2001) after a 2-month pilot study (July and August 2000) in six hospitals. The catchment population of the participating hospitals included approximately 7,400,000 residents (71% of the Portuguese population).
Isolates of N. meningitidis were directly submitted at –20ºC to the Antibiotic Resistance Unit in National Institute of Health Dr. Ricardo Jorge, Lisbon, as pure isolates. However, in some cases, only primary cultures performed at participant hospitals were sent, at 35ºC, and isolated in Antibiotic Resistance Unit. All strains were identified by standard methods (6).
The inclusion criteria for laboratory diagnosis were as follows: nonrepetitive and consecutive blood, cerebrospinal fluid (CSF) samples, or both in persons with symptoms compatible with invasive meningococcal disease. The strains from the pilot study were also included in the analysis. A case of invasive meningococcal disease was defined as disease in which N. meningitidis had been isolated by culture from two normally sterile sites (blood and CSF) in a resident of the surveillance area.
Serogroup was determined on 116 isolates by slide agglutination with the polyclonal specific rabbit antisera for A, C, X, Y, Z, W135, and 29E capsular polysaccharides of N. meningitidis and the monoclonal antibodies to determine serogroup B (Murex Diagnostic, Dartford, U.K.) (6). Serogroup findings by slide agglutination were checked by polymerase chain reaction with previously described primers (7).
For serotype and serosubtype analysis and susceptibility testing, 109 strains were available. Serotypes and subtypes were determined by an enzyme-linked immunosorbent assay method (4) by using monoclonal antibodies (RIVM, National Institute of Public Health and the Environment, the Netherlands). Serotype-specific reagents included 1, 4, 2a, 2b, 14, and 15; serosubtype-specific reagents included P1.1, P1.2, P1.4, P1.5, P1.6, P1.7, P1.9, P1.10, P1.12, P1.13, P1.14, P1.15, and P1.16.
The susceptibility to penicillin (Wyeth Lederle Portugal, Algés, Portugal) was assessed by determining MICs by using the agar dilution method with Mueller-Hinton agar supplemented with 5% sheep blood and incubated in 5% CO2 at 35°C for 24 h. N. meningitidis strains with an MIC of penicillin of <0.06 μg/mL were susceptible, strains with an MIC of penicillin of 0.12 μg/mL to 1 μg/mL had intermediate resistance to penicillin. Escherichia coli ATCC 25922 and Staphylococcus aureus ATCC 29213 were used as control strains. Production of β-lactamase was tested by nitrocefin (a chromogenic cephalosporin method).
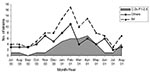
The study sample included slightly more serogroup C (58/116, 50.0%) than serogroup B (55/116, 47.4%) isolates; the rest were serogroup W135 (3/116, 2.6%). The most frequent type and subtype of serogroup B was 4:P1.15 (13.4%) and of serogroup C was 2b:P1.2,5 (75.9%) (Table). Phenotype C:2b:P1.2,5 accounted for 37.6% of all strains, but no differences existed by age and region (data not shown). Most of the 41 strains with this phenotype were isolated from November 2000 through June 2001, with a peak from February 2001 to April 2001 (Figure). This peak contributed to the higher number of isolates obtained during this period.
Strains with intermediate resistance to penicillin from serogroup B had the following serotypes and subtypes: 4:P1.15 (two strains) and one strain of each 1:P1.15, 4:P1.2,5, 14:P1.12 and NT:P1.15. Strains with intermediate resistance to penicillin from serogroup C had the following serotypes and subtypes: 2b:P1.2,5 (30 strains) and 2b:P1.2 (2 strains) and 2b:NST (2 strains). One strain from the phenotype W135:2a:P1.2,5 also showed intermediate resistance to penicillin (Table).
This study, covering approximately 71% of the Portuguese population, shows that serogroups B and C are dominant in Portugal, as they are elsewhere in Europe (1). Meningococcal disease in our study followed the usual European pattern (1), including the seasonal peak in winter and the age distribution, with children <5 years of age being the most affected group (data not shown).
B:15:P1.7,16 and B:4:P1.4 were the fourth and fifth most frequent serotype and subtypes of serogroup B in our sample, respectively, but were the major phenotypes of invasive meningococci in other European countries in 1999 and 2000, followed by B:4:P1.15, B:1:P1.14 and B:4:P1:10, in descending order (1,9). However, the most frequent serotype and subtype of serogroup B in this study was 4:P1.15 (13.4%), as in Spain (1). Spain was the only European country to report phenotype B:4:P1.15 from 1993 to 1996 (9), but it was found in the Czech Republic, Slovakia, and Malta in 1999 through 2000 (1).
Between serogroup C strains, those with serotype and subtype 2b:P1.2,5 (75.9%) were the most frequent, followed by 2b:P1.2 (7.5%) (1,9). In Europe, in 1999 through 2000, the prevalent phenotypes for strains of serogroup C were C:2a:P1.5 and C:2a:P1.2,5, followed by C:2b:P1.2,5, C:2b:P1.2, and C:2a:P1.2 (1).
The apparent endemicity of N. meningitidis C:2b:P1.2,5 in Portugal (Figure) (8), as in Spain, suggests that the features of the Iberian Peninsula are favorable for this phenotype. Invasive meningococcal disease may be caused by host factors more than bacterial determinants (10,11). Molecular analysis may be able to indicate whether the phenotype 2b:P1.2,5 is a variant of clones spreading in other countries or even a variant of previously identified clones in Portugal. Monitoring the incidence of this phenotype and its apparent emergence from 1995 (33.3%) to 2001 (75.9%) (Table) (8) is important.
The three strains of serogroup W135 in this study were all serotype and subtype 2a:P1.2,5, the predominant clone in Europe (1). This serotype was the cause of an outbreak in 2000, after the Hajj pilgrimage to Mecca (12). We have no information about contact between patients and Hajj pilgrims or the European outbreak. However, the main serotype and subtype in serogroup W135 in Portugal previously (between 1995 and 1999) was also 2a:P1.2,5 (Table).
The emergence of serogroup C, including numerous isolates with intermediate resistance to penicillin (13,14), leads us to emphasize the importance of the prophylaxis and the need for cost-benefit studies to control meningococcal disease. Resistance to penicillin can impede treatment of invasive disease, making surveillance of this resistance important. Strains of phenotypes B:4:P1.15 and C:2b:P1.2,5 most frequently had intermediate resistance to penicillin, and C:2b:P1.2,5 strains had the highest MICs of penicillin (all isolates with MIC of 0.5 μg/mL and 95% with MIC of 0.25 μg/mL). In Spain in the 1980s, types 4:P1.15 (serogroup B) and 2b (serogroup C) were also found in the main meningococci with intermediate resistance to penicillin (14).
In conclusion, continued serogrouping of meningococcal strains would be valuable because possible antigen variations caused by capsular switching (15) can occur after the period of this study, especially because of the voluntary vaccination program available in Portugal. Meningococci use this mechanism to escape control by vaccines or the natural immune protection. Consequently, the pattern of phenotypes could be subject to major changes, and adjustment to new circumstances will be needed. Antigenic characterization has contributed to the understanding of meningococcal diversity and spread of meningococcal disease. Trends were detected epidemiologically, and serotyping provided further information, which can also contribute to establishing strategies for developing a universal serogroup B vaccine. Molecular typing of N. meningitidis is also needed in Portugal to follow evolutionary changes in the bacteria and to elucidate clonal relationships between isolates.
Our results also demonstrate the importance of monitoring susceptibility to antimicrobial drugs and antigenic characteristics of meningococci; in Portugal, the prevalent phenotype C:2b:P1.2,5 is of particular concern.
Dr. Caniça is a research scientist in the Antibiotic Resistance Unit, Center of Bacteriology, at the National Institute of Health Dr. Ricardo Jorge, Lisbon, Portugal. Her research interests include emerging drug resistance and epidemiologic markers.
Acknowledgments
We thank D. Louro, P. Bajanca-Lavado, and M. Ferreira for technical support; J.-M. Alonso for kindly provided reference strains for typing; and M. Falcão for his helpful comments on the manuscript.
This study has benefited in part from financial support from Wyeth Lederle Portugal, Algés, Portugal. This work was presented in part at the Simposium WLP: Invasive pneumococcal and meningococcal infection, Lisbon, Portugal, February 2002, and at the 13th International Pathogenic Neisseria Conference, Oslo, Norway, September 2002.
References
- Noah N, Henderson B. Surveillance of bacterial meningitis in Europe 1999/2000. Communicable Disease Surveillance Centre, Public Health Laboratory Service, England; 2001.
- Peltola H. Meningococcal vaccines. Current status and future possibilities. Drugs. 1998;55:347–66. DOIPubMedGoogle Scholar
- Tikhomirov E, Santamaria M, Esteves K. Meningococcal disease: public health burden and control. World Health Stat Q. 1997;50:170–6.PubMedGoogle Scholar
- Abdillahi H, Poolman J. Whole-cell ELISA for typing Neisseria meningitidis with monoclonal antibodies. FEMS Microbiol Lett. 1987;48:367–71. DOIGoogle Scholar
- Direcção-Geral da Saúde. Estatísticas. Doenças de declaração obrigatória 1996/2000. 2001. [cited July 31, 2003]. Available from: http://www.dgsaude.pt/estat/ddo_00/ddo_96_00.htm
- World Health Organization. Laboratory methods for the diagnosis of meningitis caused by Neisseria meningitidis, Streptococcus pneumoniae and Haemophilus influenzae. 1999. [cited July 31, 2003]. Available from: http://www.who.int/emc
- Taha M-K. Simultaneous approach for nonculture PCR-based identification and serogroup prediction of Neisseria meningitidis. J Clin Microbiol. 2000;38:855–7.PubMedGoogle Scholar
- Ferreira E. Grupo de Estudos Multicêntricos da Vigilância da Susceptibilidade aos Antibióticos (GEMVSA), Caniça M. Susceptibilidade aos antibióticos e caracterização dos serogrupos de Neisseria meningitidis. Revista Portuguesa de Doenças Infecciosas. 2001;24:5–10.
- Connolly M, Noah N. Is group C meningococcal disease increasing in Europe? A report of surveillance of meningococcal infection in Europe 1993-6. Epidemiol Infect. 1999;122:41–9. DOIPubMedGoogle Scholar
- Kondaveeti S, Hibberd ML, Booy R, Nadel S, Levin M. Effect of the factor V Leiden mutation on the severity of meningococcal disease. Pediatr Infect Dis J. 1999;18:893–6. DOIPubMedGoogle Scholar
- Read RC, Camp NJ, di Giovine FS, Borrow R, Kaczmarski EB, Chaudhary AG, An interleukin-1 genotype is associated with fatal outcome of meningococcal disease. J Infect Dis. 2000;182:1557–60. DOIPubMedGoogle Scholar
- Aguilera J-F, Perrocheau A, Meffre C, Hahné S. The W135 Working Group. Outbreak of serogroup W135 meningococcal disease after the Hajj pilgrimage, Europe, 2000. Emerg Infect Dis. 2002;8:761–7.PubMedGoogle Scholar
- Ferreira E, Caniça M. Invasive meningococci with reduced susceptibility to penicillin in Portugal. J Antimicrob Chemother. 2002;49:424–5. DOIPubMedGoogle Scholar
- Sáez-Nieto JA, Lujan R, Berrón S, Campos J, Vinas M, Fusté C, Epidemiology and molecular basis of penicillin-resistant Neisseria meningitidis in Spain: a 5-year history (1985–1989). Clin Infect Dis. 1992;14:394–402.PubMedGoogle Scholar
- Swartley JS, Marfin AA, Edupuganti S, Liu L-J, Cieslak P, Perkins B, Capsule switching of Neisseria meningitidis. Proc Natl Acad Sci U S A. 1997;94:271–6. DOIPubMedGoogle Scholar
Figure
Table
Cite This Article1The hospitals and principal collaborators who participated in the Meningococci Study Group were: Hospital Dr. José Maria Grande, Portalegre (V. Inês, F. Pádua); Hospital José Joaquim Fernandes, Beja (F. Furtado, R. Bento); Hospital de Setúbal (T. Gouveia); Hospital Nossa Senhora do Rosário, Barreiro (M. Henriques, A. Jesus); Hospital Garcia de Orta, Almada (P. Azeredo, M.J. Águas, J. Diogo); Hospital Militar de Belém, Lisboa (M.T. Cabral); Hospital de Santa Maria, Lisboa (P. Valente, J. Neves, M.J. Salgado); Hospital S. Francisco Xavier, Lisboa (A. Neto, C. Lemos, F. Martins); Hospital de Dona Estefânia, Lisboa (L. Carvalho, R. Barros); Hospital Fernando Fonseca, Amadora (M.J. Brito, L. Sancho); Hospital Conde de Castro Guimarães, Cascais (M. Martins, A. Coutinho); Hospital Reynaldo dos Santos, Vila Franca de Xira (I. Fonseca, C. Tonel, M. Vasconcelos); Hospital Pediátrico-CHC, Coimbra (L. Januário); Hospital Geral dos Covões-CHC (M.J. Faria); Centro Hospitalar das Caldas da Rainha, Caldas da Rainha (C. Duarte, J. Pinto); Hospital de São Teotónio, Viseu (G. Figueiredo, L. Simões, J. Ribeiro); Hospital Padre Américo, Vale de Sousa (A. Oliveira, F. Assunção); Hospital Distrital de Aveiro, Aveiro (J. Roseta); Hospital Eduardo Santos Silva, Vila Nova de Gaia (E. Alves, P. Lopes); Hospital Geral de Santo António, Porto (J. Monteiro, J. Amorim); Hospital Joaquim Urbano, Porto (A. Horta); Hospital Distrital de Bragança, Bragança (J. Marques); Hospital S. Pedro de Vila Real, Vila Real (A. Pereira, A. Castro); Hospital Distrital de Chaves, Chaves (J. Morais); Hospital de Santa Luzia, Viana do Castelo (M. de Melo, A. Martinez); Hospital do Divino Espírito Santo, Ponta Delgada, Açores (C. Macedo, M. Mota, E. Carvalho); Centro Hospitalar do Funchal, Funchal, Madeira (M. Freitas, T. Afonso).
Table of Contents – Volume 10, Number 3—March 2004
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Manuela Caniça, Antibiotic Resistance Unit, National Institute of Health Dr. Ricardo Jorge, Av. Padre Cruz, 1649-016 Lisbon, Portugal; fax: +351217519246
Top