Volume 13, Number 4—April 2007
Dispatch
Endpoints for Lymphatic Filariasis Programs
Abstract
In 2000, annual mass administration of diethlycarbamazine and albendazole began in Leogane Commune, Haiti, to interrupt transmission of lymphatic filariasis (LF). After 5 years of treatment, microfilaremia, antigenemia, and mosquito infection rates were significantly reduced, but LF transmission was not interrupted. These finding have implications for other LF elimination programs.
Globally, more than 1 billion persons are at risk for lymphatic filariasis (LF), a mosquito-transmitted parasitic infection that causes lymphedema and hydrocele. Transmission of LF can be interrupted by annual mass treatment with drugs that target microfilariae, the stage of the parasite that circulates in the blood (1,2). Programs in Egypt, Samoa, Zanzibar, and other settings have recently completed 5 rounds of mass drug administration (MDA) (3,4), a proposed endpoint for treatment, and are now confronted with a critical question: can MDA be stopped without fear of recrudescence of LF infection?
The LF demonstration project in Leogane, Haiti, was designed as an operational research project to monitor the impact of MDA on LF infection in a high-prevalence setting. The intervention was annual MDA with diethylcarbamazine (DEC) and albendazole. We discuss how sentinel site data were used to determine whether to continue mass MDA after 5 rounds and how our experience may be relevant to other LF programs.
Leogane is located 30 km west of Port-au-Prince. Before the first MDA in 2000, 4 sentinel sites in Leogane commune were selected for annual follow-up of microfilaremia and antigenemia (5). Monitoring of filarial infection prevalence in the vector, Culex quinquefasciatus, began in these sites 3 months before the first MDA, using CDC gravid traps (Model 1712, J.W. Hock Co., Gainesville, FL, USA) (6); testing continued on a semimonthly basis. Infected mosquitoes were defined as those carrying microfilariae or larvae (L1–L3); L3 were the infectious larval stage. Protocols for collecting data from sentinel sites were approved by the Centers for Disease Control and Prevention Institutional Review Board and the Ethics Committee at Hopital Ste. Croix.
In October 2000 and every October thereafter, DEC (6 mg/kg) and albendazole (400 mg; GlaxoSmithKline, Brentford, UK) were co-administered at stationary posts to persons >2 years of age, excluding pregnant women and persons too ill to receive the drugs. Adverse events were monitored each year by recording the number of persons who returned to distribution posts with complaints. Cluster surveys were conducted after the first and third MDA to assess coverage and the effect of health messages on compliance (7,8).
[[AA:T1:PREVIEWHTML]]Reported coverage in 2000–2004 for MDAs 1–5 was 69%, 50%, 84%, 89%, and 104%, respectively (Table). Decreased coverage in 2001 may have been related to a relatively high incidence of adverse events caused by death of microfilariae and adult worms during the first MDA (9). The increase in reported coverage in 2004 may have been due to an influx of displaced persons from areas of Haiti affected by civil strife. Survey-based coverage in 2000 and 2002 was 71% and 79%, respectively (7,8). Adverse events diminished with each year of treatment, from 23.1% of persons treated during 2000 to 3% during 2004 (p<0.0001).
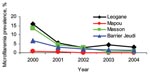
Baseline microfilaremia prevalence rates were 0.8%, 7%, 12%, and 16% in the sentinel sites of Mapou, Barrier-Jeudi, Masson-Mathieu, and Leogane, respectively (Figure 1). Microfilaremia prevalence decreased significantly in each of the sentinel sites (Mapou, p = 0.0291; each of the other sites, p<0.0001). Antigenemia prevalence declined less dramatically, by 18.6%, 34.6%, 74.2%, and 54.7% in Mapou, Barrier Jeudi, Masson-Mathieu, and Leogane, respectively (p<0.0001 in all sites except Mapou).
Baseline mosquito infection rates 3 months before the first MDA were 0.5%, 2.9%, 3.5%, and 4.0% in Mapou, Masson-Mathieu, Leogane, and Barrier-Jeudi, respectively. After MDA 1, infection prevalence decreased significantly only in Masson-Mathieu (p = 0.004); however, after 2 rounds of MDA, infection was reduced significantly at all sites (p<0.007) except Mapou (Figure 2). After MDA 4, infection prevalence was 0% during some months at all sentinel sites, although infected mosquitoes were detected sporadically at all sites but Mapou. The prevalence of infective mosquitoes was lower than the prevalence of infected mosquitoes (p<0.05), but parallel declines were observed after MDA (data not shown).
These data were collected to monitor progress and to provide a basis for programmatic decisions. In January 2005, 3 months after MDA 5, a meeting was convened in Leogane with program and ministry staff to discuss the need for further MDA. Sustained reductions in LF infection in both humans and mosquitoes demonstrated the substantial effects of the intervention through 4 MDA rounds. However, persistent antigenemia and sporadic parasitemia were detected at all sentinel sites. Project leaders adopted a conservative approach and planned for MDA 6 on the basis of the evidence of continued transmission in the sentinel sites.
Several factors supported this decision, including detection of infections in both humans and mosquitoes and concerns about systematic noncompliance (8), the potential for inflated coverage estimates due to population migration, the nonrepresentativeness of sentinel sites for estimating MDA impact, and the insensitivity of blood smears for monitoring microfilaremia. Since the cost of an additional MDA was not prohibitive, project staff decided that the evidence of continued transmission, the health benefits of mass treatment to the community, and the risk of stopping treatment prematurely justified a sixth round of MDA in October 2005. Results from Leogane and other programs have demonstrated that 5 rounds of MDA may not be sufficient to interrupt transmission when baseline antigenemia is high, whereas in low-prevalence areas <5 rounds appears to be adequate (3). Mathematical models as well as program experience suggest that the number of MDAs required depends on baseline intensity of infection, assuming adequate coverage (10,11).
Adequate monitoring data are important for making decisions regarding continuation of mass treatment. Microfilaremia and ICT testing are the gold standards for measuring the impact of MDA; however, nocturnal blood collection required for microfilaria testing is inconvenient, the high cost of the ICT is a concern (≈$2.65), and the sensitivity of both tests decreases as LF intensity and prevalence decline.
Entomologic monitoring provides an alternative method of measuring the impact of MDA on transmission. Although it circumvents the human cost of repeated blood collection and provides a direct, real-time measure of potential transmission, continuous mosquito collection and dissection were more costly and labor-intensive than other monitoring methods that we used. Conducting intermittent rather than continuous collections may be an alternative approach.
The limitations of these monitoring tools highlight the need for more sensitive, standardized tools to help programs define MDA endpoints and to conduct surveillance. Antibody responses may develop before patent infection and serve as a cumulative measure of filarial exposure and a proxy for transmission (12). In Egypt, antibody surveys of children beginning school were used to monitor for incident exposure, indicative of ongoing transmission (3). Additional studies are needed to validate antibody tests and to analyze the relationship between antibody prevalence and transmission intensity.
In summary, MDA-based LF programs, including that in Leogane, lead to dramatic declines in filarial infection in humans and mosquitoes after several annual rounds of MDA (2,3,13–15). The outcomes of the Leogane project and others that have completed 5 rounds of MDA strongly suggest that the duration of treatment is related to the baseline transmission intensity and infection prevalence. Several issues—population migration, systematic noncompliance, and sentinel site bias—have emerged as variables that complicate decision making. Investigating their effect on infection and transmission in an operational context is critical.
Ms. Grady joined the Division of Parasitic Diseases, CDC, in Atlanta, Georgia as an Emerging Infectious Diseases Training Fellow. She is attending the University of Washington School of Medicine.
Acknowledgments
We thank Jack Guy Lafontant and the staff of the Leogane demonstration project at Hopital Ste. Croix, Leogane, Haiti, for their support and the residents of the sentinel sites who volunteered for testing over the years.
This project was funded by the CDC Emerging Infectious Diseases funds and by a grant from the Bill & Melinda Gates Foundation awarded to the University of Notre Dame, Indiana.
This article is dedicated to the memory of Jean Joseph Dorvil, a program administrator who was killed in Port-au-Prince in December 2004.
References
- Ottesen EA, Duke BO, Karam M, Behbehani K. Strategies and tools for the control/elimination of lymphatic filariasis. Bull World Health Organ. 1997;75:491–503.PubMedGoogle Scholar
- World Health Organization. Global programme to eliminate lymphatic filariasis: progress report on mass drug administrations in 2005. Wkly Epidemiol Rec. 2006;81:221–32.PubMedGoogle Scholar
- Ramzy RMR, El Setouhy M, Helmy H, Ahmed ES, Abd Elaziz KM, Farid HA, Effect of yearly mass drug administration with diethylcarbamazine and albendazole on bancroftian filariasis in Egypt: a comprehensive assessment. Lancet. 2006;367:992–9. DOIPubMedGoogle Scholar
- Mohammed KA, Molyneux DH, Albonico M, Rio F. Progress toward eliminating lymphatic filariasis in Zanzibar: a model programme. Trends Parasitol. 2006;22:340–4. DOIPubMedGoogle Scholar
- de Rochars MB, Kanjilal S, Direny AN, Radday J, Lafontant JG, Mathieu E, The Leogane, Haiti demonstration project: decreased microfilaremia and program costs after three years of mass drug administration. Am J Trop Med Hyg. 2005;73:888–94.PubMedGoogle Scholar
- Goodman DS, Orelus JN, Roberts JM, Lammie PJ, Streit T. PCR and mosquito dissection as tools to monitor filarial infection following mass treatment. Filaria Journal [serial online]. 2003 July; 2(11): [about 9 p.]. Available from http://www.filariajournal.com/content/2/1/11.
- Mathieu E, Deming M, Lammie PJ, McLaughlin SI, Beach MJ, Deodat DJ, Comparison of methods for estimating drug coverage for filariasis elimination, Leogane Commune, Haiti. [PMID: 15307410]. Trans R Soc Trop Med Hyg. 2003;97:501–5. DOIPubMedGoogle Scholar
- Mathieu E, Direny A, Beau de Rochars M, Streit T, Addiss DG, Lammie PJ. Participation in three consecutive mass drug administrations in Leogane, Haiti. Trop Med Int Health. 2006;11:862–8. DOIPubMedGoogle Scholar
- McLaughlin SI, Radday J, Michel MC, Addiss DG, Beach MJ, Lammie PJ, Frequency, severity, and costs of adverse reactions following mass treatment for lymphatic filariasis using diethylcarbamazine and albendazole in Leogane, Haiti, 2000. Am J Trop Med Hyg. 2003;68:568–73.PubMedGoogle Scholar
- Stolk WA, Swaminathan S, van Oortmarssen GJ, Das PK, Habbema JD. Prospects for elimination of bancroftian filariasis by mass drug treatment in Pondicherry, India: A simulation study. J Infect Dis. 2003;188:1371–81. DOIPubMedGoogle Scholar
- Michael E, Malecela-Lazaro MN, Simonsen PE, Pedersen EM, Barker G, Kumar A, Mathematical modeling and the control of lymphatic filariasis. Lancet Infect Dis. 2004;4:223–33. DOIPubMedGoogle Scholar
- Lammie P, Weil G, Noordin R, Kaliraj P, Steel C, Goodman D, Recombinant antigen-based antibody assays for the diagnosis and surveillance of lymphatic filariasis - a multicenter trial. Filaria Journal [serial online]. 2004;3(9). Available from http://www.filariajournal.com/content/3/1/9.
- Bockarie MJ, Tisch DJ, Kastens W, Alexander ND, Dimber Z, Bockarie F, Mass treatment to eliminate filariasis in Papua New Guinea. N Engl J Med. 2002;347:1841–8. DOIPubMedGoogle Scholar
- Ramaiah KD, Das PK, Vanamail P, Pani SP. The impact of six rounds of single-dose mass administration of diethylcarbamazine or ivermectin on the transmission of Wuchereria bancrofti by Culex quinquefasciatus and its implications for lymphatic filariasis elimination programmes. Trop Med Int Health. 2003;8:1082–92. DOIPubMedGoogle Scholar
- Richards FO Jr, Pam DD, Kal A, Gerlong GY, Onyeka J, Sambo Y, Significant decrease in the prevalence of Wuchereria bancrofti infection in anopheline mosquitoes following the addition of albendazole to annual ivermectin-based, mass treatments in Nigeria. Ann Trop Med Parasitol. 2005;99:155–64. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 13, Number 4—April 2007
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Patrick J. Lammie, Division of Parasitic Diseases, Centers for Disease Control and Prevention, 4770 Buford Hwy NE, Mailstop F-13, Bldg 23, Room 1021, Atlanta, GA 30341, USA;
Top