Volume 15, Number 3—March 2009
Dispatch
Sudden Increases in Listeriosis Rates in England and Wales, 2001 and 2003
Abstract
The monthly incidence of listeriosis infections in England and Wales had 2 sudden increases during April 2001 (41%) and March 2003 (48%). Although no causative association is demonstrated, these increases correspond to key dates relating to the onset and aftermath of the 2001 foot and mouth disease outbreak in the United Kingdom.
Prevention of listeriosis (infection caused by Listeria monocytogenes) is a serious food safety issue, particularly for pregnant women, the elderly, and those who are immunocompromised. Death occurs in 20%–30% of cases, making listeriosis a leading cause of food poisoning deaths in Europe and the United States (1). An increasing rate of listeriosis has been reported in several European countries (2). Our study focused on the large increase in the number of reported listeriosis cases in England and Wales during 2 months in separate years (April 2001 and March 2003). These increases were permanent and cumulative; after each increase, monthly incidence of listeriosis did not return to previous levels. These increases primarily reflect a higher rate of bacteremic listeriosis in those >60 years of age and are not otherwise correlated with geography, gender, ethnicity, socioeconomic factors, or infectious serotypes (3).
We compared monthly listeriosis data from England and Wales with temperature records from 1989 through 2007 to determine the influence of various potential predictors on the number of listeriosis cases. UK Health Protection Agency (HPA) data listing total monthly cases of human listeriosis in England and Wales during 1990–2007 (4,5) are aggregate. All age categories and regions were included and were collated by the HPA Centre for Infections from voluntary reporting by microbiology laboratories and from referrals of cultures. These publicly available data were also validated by the HPA, and in our analysis we used revised figures based on that validation. Our analysis covered the period from 1990, when active surveillance of listeriosis began, through 2007. Pregnancy-associated cases (mother and neonate) were counted as 1 case. Undated cases that could not be assigned to a particular month were excluded from analysis. We used the UK Met Office mean monthly area temperature time series for 1989–2007 and 30-year means averaged during 1961–1990 (6).
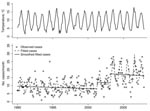
Exploratory linear regression analyses suggested a positive correlation between the number of listeriosis cases and the monthly mean UK ambient temperature, as well as suggesting a change in this relationship after 2000 (p = 0.001; Figure 1, panel A). However, residual variability was not constant, and the monthly counts are likely to be overdispersed due to clustering of cases (3). The data were fitted again by using a negative binomial generalized linear model with a logarithmic link function, a common model for time series of foodborne illness cases (7,8). To separate seasonality of listeriosis rates from dependence on temperature, we considered the 30-year mean monthly temperatures from 1961–1990, as well as monthly temperature anomalies (observed mean temperature minus 30-year mean). To determine whether temperatures could have a delayed effect on listeriosis incidence, we also included mean and anomaly temperature variables lagged by 1 or more months. To allow for 2 break points at which the incidence of listeriosis may have suddenly changed, dummy variables were used to represent periods before, between, and after the months in which these increases might have occurred. A best-fit model was selected according to the corrected Akaike Information Criterion (AIC) (9) by using stepwise regression at all combinations of 2 break point months from January 1996 through December 2007. To examine changing effects on incidence, interactions between break point indicators and other variables were considered, even if the main effects were not yet in the model. Main effects were subsequently added to the final model if any interaction terms were included.
The best-fit model included 2 break points (Tables 1, 2; Figure 1, panel B; Figure 2). The overall rate of cases increased by 40.83% in April 2001 (adjusted p = 0.001, 95% confidence interval [CI] 17.29%–68.93%); a further increase of 47.76% occurred in March 2003 (adjusted p<0.001, 95% CI 27.92%–71.13%). According to the corrected AIC, there is statistical evidence of changes in the incidence of listeriosis in a range of months around these best-fit values, and weak support for a change in early 2005, apparently due to low numbers of cases in the first months of that year and the following winter (Figure 1, panel B). Most of the seasonality in the number of cases was accounted for by the 30-year mean monthly temperatures. Each extra degree Celsius of mean monthly temperature corresponded to a 2.42% increase in cases in the current month (adjusted p = 0.044, 95% CI, 0.55%–4.33%) and a 4.09% increase in the following month (adjusted p<0.001, 95% CI 2.19%–6.03%). The 1-month lag reflects delays between food production and consumption plus the known long incubation of listeria infections. Similar lags have been observed for other enteric pathogens (6,11). A relationship also appears to exist between the rate of listeriosis and the 1-month lagged temperature anomaly starting in April 2001, which corresponded to an additional 5.71% of listeriosis cases per degree Celsius (95% CI –2.10%–14.15%) when compared with the main effect of temperature anomaly in 1990–2007. This increase was not significant (adjusted p = 0.312), although the power of this test is only ≈15% at an adjusted significance level of 0.05 (post hoc power analysis performed by computer simulation of the fitted model in the R statistical computing environment). The model also includes a slight negative trend in cases over time (–0.13% per month, 95% CI –0.26%–0.01%), but evidence for this trend is very weak (adjusted p = 0.188).
The changes in the incidence of listeriosis appear to have been quite sudden (Figure 2). Causative explanations based on gradual demographic or behavioral changes have previously been ruled out (3), and those based on dynamic processes seem unlikely because no evidence exists for epidemiologic feedback between the source of infections and clinical cases. One possibility is that the increases are due to contamination of a small number of food products, as has been suggested as an explanation for an upsurge in listeriosis rates in the late 1980s. However, a restricted range of strains was responsible for most of the additional cases at that time (12), and no evidence exists of such a pattern since 2001 (3). An alternative possibility is that the phenomenon is a consequence of changes in government policy or business practices that have had more widespread effects on food processing, distribution, or preparation.
We found notable coincidences between the dates of the increases in listeriosis infection rates and the dates of events associated with the 2001 foot and mouth disease (FMD) outbreak in the United Kingdom. The April 2001 increase in listeriosis rates occurred shortly after the outbreak of FMD in February 2001, allowing for a delay similar to the incubation period of listeria infections. The March 2003 increase in listeriosis rates occurred in the same month as the relaxation of movement restrictions on livestock instituted after the 2001 FMD outbreak (13). The diverse and widespread consequences of the 2001 FMD outbreak are well-documented (14,15), and it seems plausible that such major disturbances to agricultural production could be the ultimate cause of the large increases in listeriosis rates that have been observed. The coincidence of these events raises the possibility that the change in listeriosis rates would be an unrecognized outcome of the 2001 UK FMD crisis, although we caution that our analysis of the of these cases does not demonstrate whether a causative link exists.
Listeriosis incidence in England and Wales has increased notably since the beginning of 2001, with 2 separate, sudden increases recorded in April 2001 and March 2003. Gillespie et al. argue that blame for these increases cannot be ascribed to any of a variety of specific factors (3). Instead, more widespread changes affecting food production, processing, or consumption could be the root of the problem. Incidence of this serious disease has risen substantially in England and Wales, and an understanding of why will be important for management of listeriosis as a public health issue.
Dr Cairns was a postdoctoral research assistant in the School of Biological Sciences at the University of Bristol when this work was performed and is now a research scientist in the Cancer Epidemiology Unit, University of Oxford. His research interests are statistical and mathematical approaches to epidemiology, ecology, and population biology.
Dr Payne is a Royal Society University Research Fellow in the School of Biological Sciences at the University of Bristol. His main research interest is the application of nonlinear dynamical systems theory to biology, including studies of evolutionary ecology, pathogen dynamics, and population biology.
Acknowledgments
We thank the UK HPA and the UK Met Office for sharing the data used in this study. We are grateful for discussions with Vincent Jansen, Victoria Cairns, and the following members of the Health Protection Agency, London: Iain Gillespie, Kathie Grant, Christopher Lane, Christine Little, and Jim McLauchlin. We also thank the anonymous reviewers for valuable comments.
This work was supported by a grant from the Biotechnology and Biological Sciences Research Council and UK Food Standards Agency (grant no. BB/C504578/1).
References
- de Valk H, Jacquet C, Goulet V, Vaillant V, Perra A, Desenclos J-C, ; Listeria Working Group. Feasibility study for a collaborative surveillance of Listeria infections in Europe; report to the European Commission. Paris: DGSANCO; Mar 2003 [cited 2008 Jul 8]. Available from http://www.invs.sante.fr/publications/2004/listernet/rap_listernet_p1_76.pdf
- Koch J, Stark K. Significant increase of listeriosis in Germany–—epidemiological patterns 2001–2005. Euro Surveill. 2006;11:85–8.PubMedGoogle Scholar
- Gillespie IA, McLauchlin J, Grant KA, Little CL, Mithani V, Penman C, Changing pattern of human listeriosis, England and Wales, 2001–2004. Emerg Infect Dis. 2006;12:1361–6.PubMedGoogle Scholar
- Health Protection Agency. Cases: England and Wales, by month, 1990–2006: Listeria monocytogenes, human cases in residents of England and Wales by month reported to the Health Protection Agency Centre for Infections 1990–2006. 2008 [cited 2008 Jul 8]. Available from http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1195733767791
- Health Protection Agency. Health protection report. Advice to pregnant women during the lambing season. 25 Jan. 2008;2(4) [cited 2008 Jul 8]. Available from http://www.hpa.org.uk/hpr/archives/2008/news0408.htm
- UK Met Office. UK mean temperature (degrees C) areal series, starting from 1914 [database on the Internet]. UK Met Office; 2007 [updated monthly; cited 2007 May 31]. Available from http://www.metoffice.gov.uk/climate/uk/seriesstatistics/uktemp.txt
- D’Souza RM, Becker NG, Hall G, Moodie KB. Does ambient temperature affect foodborne disease? Epidemiology. 2004;15:86–92. DOIPubMedGoogle Scholar
- Tam CC, Rodrigues LC, O’Brien SJ, Hajat S. Temperature dependence of reported campylobacter infection in England, 1989–1999. Epidemiol Infect. 2006;134:119–25. DOIPubMedGoogle Scholar
- Burnham KP, Anderson DR. Model selection and multi-model inference, 2nd ed. New York: Springer; 2003.
- Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70.
- Bentham G, Langford IH. Climate change and the incidence of food poisoning in England and Wales. Int J Biometeorol. 1995;39:81–6. DOIPubMedGoogle Scholar
- McLauchlin J, Hall SM, Velani SK, Gilbert RJ. Human listeriosis and paté: a possible association. BMJ. 1991;303:773–5.PubMedGoogle Scholar
- Madders B. Review of the livestock movement controls. Department for Environment, Food and Rural Affairs (UK); July 2006 [cited 2008 July 8]. Available from http://www.defra.gov.uk/animalh/id-move/pdf/livestock_movement_controls-review.pdf
- The Royal Society. Infectious diseases in livestock. London: The Society; July 2002 [cited 2008 Jul 8]. Available from http://royalsociety.org/inquiry/index/intro.htm
- Anderson I. Foot and mouth disease 2001: lessons to be learned inquiry report. London: The Stationery Office; July 2002 [cited 2008 Jul 8]. Available from http://archive.cabinetoffice.gov.uk/fmd/index.htm
Figures
Tables
Cite This ArticleTable of Contents – Volume 15, Number 3—March 2009
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Benjamin J. Cairns, Cancer Epidemiology Unit, University of Oxford, Richard Doll Building, Oxford OX3 3LF, UK;
Top