Volume 15, Number 5—May 2009
Dispatch
Human Streptococcus agalactiae Isolate in Nile Tilapia (Oreochromis niloticus)
Abstract
Streptococcus agalactiae, the Lancefield group B streptococcus (GBS) long recognized as a mammalian pathogen, is an emerging concern with regard to fish. We show that a GBS serotype Ia multilocus sequence type ST-7 isolate from a clinical case of human neonatal meningitis caused disease and death in Nile tilapia (Oreochromis niloticus).
Streptococcus agalactiae, group B streptococcus (GBS), has a broad host range and is pathogenic to mammals, reptiles, amphibians, and fish (1). This organism has also been identified in aquatic mammals, both captive and wild bottlenose dolphins (Tursiops truncatus) (2,3). GBS causes mastitis in cattle and meningitis in human neonates (4). It also causes meningoencephalitis in fish (5,6). Since the first report of GBS in hatchery-reared freshwater fish in the United States in 1966 (7), reports of piscine GBS have increased. Piscine GBS, like human and bovine GBS, is found worldwide and affects a variety of freshwater and marine fish under a broad spectrum of environmental conditions (6,8).
Sustained emergence of human GBS neonatal disease for undetermined reasons has spurred many GBS genomic diversity studies. Acquisition of bovine GBS by humans has been proposed as 1 plausible explanation (9). Human and bovine GBS isolates have been considered genetically distinct populations (10) and as related populations arising from a common ancestor, presumably bovine (1,9).
Two lineages of bovine GBS (multilocus sequence type ST-23 and ST-61) appear to have a genetic relationship with human GBS. Human serotype Ia strains in the ST-23 lineage and human serotype III ST-17 strains are related to bovine ST-61 strains and frequently associated with neonatal infections (10,11). Phylogenetic studies have focused on homogeneity or heterogeneity of lineages and association with carried or invasive GBS. Many researchers believe that GBS serotype does not correlate with evolutionary relationships. Strains of different serotypes and sequence types often share more genes than strains of the same serotype and contain carried and invasive strains, traits suggestive of opportunistic pathogenicity (9,11,12).
Whether GBS is a zoonotic organism has not been adequately explored. Conclusions of genomic studies can only infer virulence, infectivity, and transfer between different animals on the basis of serologic, molecular, and computational analyses of GBS isolates. Bovine GBS isolates of unknown sequence type were not infective for Nile tilapia (Oreochromis niloticus) (13). However, potential for infection between homothermic hosts and poikilothermic animals has been demonstrated.
GBS transmission from mice to reptiles occurs by oral ingestion (14). In tilapia (mean weight 40 g) infectivity studies with a dolphin GBS isolate, disease signs and a mortality rate of 90% were noted within 6 days postinoculation with 107 CFU/fish (3). Piscine, dolphin, and human GBS isolates have been reported (15) to share the same serotype (Ia) and sequence type (ST-7) as that reported from human GBS carried (strain from a person with no evidence of disease) and neonatal invasive strains from Japan (4) and North America (isolate A909) (11). This finding indicates that piscine and dolphin GBS isolates may have been derived from human sources and caused a fish epidemic in Kuwait and that serotype Ia ST-7 GBS may cause a zoonosis (15). Non–ST-7 fish isolates are widely divergent from other animal GBS isolates (12,15). We conducted a study of experimentally induced infection to determine whether a human serotype, Ia ST-7 GBS isolate, could cause disease signs and death in fish.
Nile tilapia served as experimental fish because they could be held at warm water temperatures closer to the normal human body temperature of 37°C than other available fish species. Seven groups of 10 tilapia (mean ± SE weight 28.20 ± 0.51 g) each were housed in 57-L aquariums at the Aquatic Animal Health Research Laboratory (Chestertown, MD, USA). All tanks were supplied with flow-through dechlorinated tap water and 2 submersible heaters and air stones to maintain desired water temperature and dissolved oxygen (DO) levels. Water quality (mean ± SE temperature, DO, and ammonia concentration) was measured daily by using a YSI 85 meter (Yellow Springs Instrument Co., Yellow Springs, OH, USA) and a Fresh Water Aquaculture Kit (Model AG-2; LaMotte Company, Chestertown, MD, USA). Temperature was 32.1 ± 0.09°C, DO was 4.2 ± 0.14 mg/L, and ammonia concentration was 0.74 ± 0.08 mg/L. Fish were fed daily (4% of bodyweight) with Aquamax Grower 400 fish feed (Purina, Brentwood, MO, USA) and maintained and handled according to Institutional Animal Care and Use Committee–approved guidelines.
The serotype Ia ST-7 human GBS isolate (ID# 510012) was obtained from a patient in Japan who had neonatal meningitis. The isolate was cultured overnight on 5% sheep blood agar (SBA; Remel, Lenexa, KS, USA) at 32°C. Before the study, the isolate was passed through 5 Nile tilapia (weight 18.4 ± 0.48 g) 1 time each by intraperitoneal injection of 107 CFU of GBS/fish. Specimens from a fish that died 3 days postchallenge were cultured on SBA, and GBS was recovered from nostrils, intestines, posterior kidney, and brain. One GBS colony isolated from brain was cultured on SBA, typed as GBS by Lancefield grouping (6), and used for experimental infection.
Serial dilutions of the GBS isolate were prepared in tryptic soy broth (TSB; Remel), and 10 fish (weight 28.2 ± 0.51 g) were each injected intraperitoneally with 0.1 mL of inoculum at 107, 106, 105, 104, 103, or 102 CFU/fish. Ten control fish were injected with 0.1 mL of TSB only. Fish were placed in separate 57-L aquariums at 32°C according to dose and monitored daily for signs of disease and death for 14 days postchallenge. Moribund fish were humanely euthanized by an overdose of tricaine methanesulfonate (MS-222; Argent Chemical Laboratories, Redmond, WA, USA).
Bacterial samples were obtained from nostrils and brains of all moribund or dead fish and cultured on SBA at 32°C for 24 h for GBS. Identification of GBS was performed by using methods of Evans et al. (6) and the BIOLOG MicroLog3 Microbial Identification System (BIOLOG, Hayward, CA, USA) according to the manufacturer’s instructions. BIOLOG results were compared with a Microlog database (www.biolog.com/mID_product.html); a similarity index >0.50 and high probability (>90%) were considered a strong confirmation for GBS.
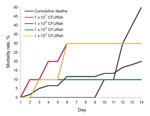
Within 7 days postchallenge, the 102, 103, and 107 CFU/fish groups had a mean cumulative mortality rate of 11.7% (7/60) (Figure). Overall, deaths occurred on day 2 and the mortality rate reached 20% after 14 days of observation. Deaths after day 10 occurred in fish that received 106 CFU. Sampled organs were negative for GBS and deaths were attributed to tank mate aggression to weakened fish. A linear dose response was not seen. Deaths occurred at low (102–103 CFU/fish) and high (107 CFU/fish) doses but not at median doses (Table). Disease signs in tilapia exposed to human GBS were lethargy, anorexia, dark coloration, opaque eyes, and remaining stationary at the bottom of the tank.
All sampled organs from fish dying within 7 days of infection contained β-hemolytic, gram-positive, oxidase-negative, catalase-negative bacteria. BIOLOG analysis confirmed identification as GBS (similarity index 0.79, probability 100%). None of the TBS-injected control fish showed signs of disease or died.
Deaths among experimentally infected Nile tilapia indicate that an Ia ST-7 human GBS isolate can be pathogenic to fish. Such isolates have been associated with human (4,12) and fish disease as well as with a marine mammal sampled during a GBS fish kill (15). The human isolate was virulent in tilapia at 102, 103, 106, and 107 CFU/fish, and GBS was reisolated from diseased fish. These experimental findings suggest GBS transmission between mammals and fish and that GBS-induced fish epidemics can originate from mammalian sources. Although we studied only 1 human isolate, other isolates or isolates repeatedly passed through fish may be more virulent. Susceptibility to GBS may also be enhanced by suboptimal environmental conditions, such as low DO, high ammonia levels, euthrophication, harmful algae, and changing or extreme water temperatures (5,6). Future histopathologic investigations may characterize the distribution and nature of the host response to human GBS.
Dr Evans is an aquatic pathobiologist at the Aquatic Animal Health Research Laboratories of the Agricultural Research Service in Chestertown, Maryland. Her primary research interests include fish vaccinology and bacterial pathogenesis.
Acknowledgment
We thank Shinji Takahashi for providing the human GBS isolate, Daniel Brougher for technical assistance, and Lisa Biggar for editing the manuscript.
References
- Elliott JA, Facklam RR, Richter CB. Whole-cell protein patterns of nonhemolytic group B, type1b, streptococci isolated from humans, mice, cattle, frogs, and fish. J Clin Microbiol. 1990;28:628–30.PubMedGoogle Scholar
- Zappulli V, Mazzariol S, Cavicchiolo L, Petterino C, Bargelloni L, Castagnaro M. Fatal necrotizing fasciitis and myositis in a captive common bottlenose dolphin (Tursiops truncatus) associated with Streptococcus agalactiae. J Vet Diagn Invest. 2005;17:617–22.PubMedGoogle Scholar
- Evans JJ, Pasnik DJ, Klesius PH, Al-Ablani S. First report of Streptococcus agalactiae and Lactococcus garvieae from a wild bottlenose dolphin (Tursiops truncatus). J Wildl Dis. 2006;42:561–9.PubMedGoogle Scholar
- Jones N, Bohnsack JF, Takahashi S, Oliver KA, Chan M-S, Kunst F, Multilocus sequence typing system for group B streptococcus. J Clin Microbiol. 2003;41:2530–6. DOIPubMedGoogle Scholar
- Eldar A, Bejerano Y, Livoff A, Horovitcz A, Bercovier H. Experimental streptococcal meningo-encephalitis in cultured fish. Vet Microbiol. 1995;43:33–40. DOIPubMedGoogle Scholar
- Evans JJ, Klesius PH, Glibert PM, Shoemaker CA, Al Sarawi MA, Landsberg J, Characterization of beta-haemolytic group B Streptococcus agalactiae in cultured seabream, Sparus auratus (L.), and wild mullet, Liza klunzingeri (Day), in Kuwait. J Fish Dis. 2002;25:505–13. DOIGoogle Scholar
- Evans JJ, Klesius PH, Shoemaker CA. An overview of Streptococcus in warmwater fish. Aquaculture Health International. 2006;7:10–4.
- Bisharat N, Crook DW, Leigh J, Harding RM, Ward PN, Coffey TJ, Hyperinvasive neonatal group B streptococcus has arisen from a bovine ancestor. J Clin Microbiol. 2004;42:2161–7. DOIPubMedGoogle Scholar
- Bohnsack JF, Whiting AA, Martinez G, Jones N, Adderson EE, Detrick S, Serotype III Streptococcus agalactiae from bovine milk and human neonatal infections. Emerg Infect Dis. 2004;10:1412–9.PubMedGoogle Scholar
- Tettelin H, Masignani V, Cieslewicz MJ, Donati C, Medini D, Ward NL, Genome analysis of multiple pathogenic isolates of Streptococcus agalactiae: implications for the microbial “pan-genome.”. Proc Natl Acad Sci U S A. 2005;102:13950–5. DOIPubMedGoogle Scholar
- Brochet M, Couvé E, Zouine M, Vallaeys T, Rusniok C, Lamy M-C, Genomic diversity and evolution within the species Streptococcus agalactiae. Microbes Infect. 2006;8:1227–43. DOIPubMedGoogle Scholar
- Garcia JC. A comparative investigation of Streptococcus agalactiae isolates from fish and cattle [doctoral dissertation]. Auburn (AL): Auburn University; 2007.
- Hetzel U, König A, Yildirim AÖ, Lämmler C, Kipar A. Septicaemia in emerald monitors (Varanus prasinus Schlegel 1839) caused by Streptococcus agalactiae acquired from mice. Vet Microbiol. 2003;95:283–93. DOIPubMedGoogle Scholar
- Evans JJ, Bohnsack JF, Klesius PH, Whiting AA, Garcia JC, Shoemaker CA. Phylogenetic relationships among Streptococcus agalactiae isolated from piscine, dolphin, bovine, and human sources: a dolphin and piscine lineage associated with a fish epidemic in Kuwait is also associated with human neonatal infections in Japan. J Med Microbiol. 2008;57:1369–76. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 15, Number 5—May 2009
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Joyce J. Evans, Agricultural Research Service, US Department of Agriculture, 118B Lynchburg St, Chestertown, MD 21620, USA
Top