Volume 20, Number 8—August 2014
Letter
Decline in Japanese Encephalitis, Kushinagar District, Uttar Pradesh, India
To the Editor: Kakkar et al. recently concluded that the low-quality surveillance data on acute encephalitis syndrome (AES)/Japanese encephalitis (JE) in Kushinagar District, India, provide little evidence to support development of prevention and control measures and to estimate the effect of interventions (1). Analysis of the surveillance data, however, does provide evidence supporting the effect of an ongoing intervention (i.e., JE vaccination).
In accordance with the surveillance protocol, cerebrospinal fluid and/or serum samples from AES patients admitted to the Baba Raghav Das Medical College (Gorakhpur, India) are tested for IgM against JE at the field laboratory of National Institute of Virology (NIV) at Gorakhpur (2). The samples are tested by using the ELISA developed by NIV Pune (Pune, India), which has a specificity of 85% (range 77%–95%) and sensitivity of 71% (range 71%–75%) (3). Patients with samples negative for JE are considered to have JE-negative AES.
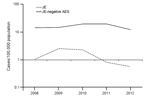
We obtained the line-list of AES patients from the NIV laboratory at Gorakhpur for 2008–2012. Analysis of the surveillance data indicated that 251 (8.2%, range 4%–14.7%) of the 3,047 AES patients from Kushinagar were positive for JE IgM and therefore considered to be JE case-patients. JE incidence per 100,000 persons in the district declined from 2.3 cases in 2010 to 0.81 in 2011 to 0.58 in 2012 (Figure). The decline in JE incidence since 2010 could be a consequence of JE vaccination activities in Kushinagar. In 2010, a mass vaccination campaign with 1 dose of JE vaccine (SA 14–14–2 strain) was conducted among children 1–15 years of age. Subsequently, the vaccine was introduced into the childhood vaccination program as a 1-dose strategy in 2011 and a 2-dose strategy in 2013. Unfortunately, information about evaluated coverage of JE vaccine is not available from the district. On the other hand, the average annual incidence of JE-negative AES during the same period was 16 cases per 100,000 persons (95% CI 14.8–17.2), and this incidence has remained relatively stable since 2008.
With the isolation of enteroviruses from JE-negative AES patients, waterborne transmission has been hypothesized, and the focus of intervention has shifted toward improving sanitation and water quality. However, enteroviruses were detected only in a small proportion of AES patients. Although the quality of AES surveillance needs to be improved, as Kakkar et al. suggested (1), further studies are needed to understand the etiology of JE-negative AES in the district and the risk factors for transmission. These studies might include systematically investigating patients and environmental samples for enteroviral and other etiologic agents.
References
- Kakkar M, Rogawski ET, Abbas SS, Chaturvedi S, Dhole TN, Hossain SS, Acute encephalitis syndrome surveillance, Kushinagar District, Uttar Pradesh, India, 2011–2012. Emerg Infect Dis. 2013;19:1361–7 . DOIPubMedGoogle Scholar
- Directorate of National Vector Borne Diseases Control Programme. Guidelines for surveillance of acute encephalitis syndrome (with special reference to Japanese encephalitis) [cited 2013 Sep 11]. http://www.nvbdcp.gov.in/Doc/AES%20guidelines.pdf
- World Health Organization Regional Office for Southeast Asia. Fourth bi-regional meeting on the control of Japanese encephalitis. Report of the meeting Bangkok, Thailand, 7–8 June 2009 [cited 2013 Aug 15]. http://www.wpro.who.int/immunization/documents/docs/JEBiregionalMeetingJune2009final.pdf
Figure
Cite This ArticleRelated Links
Table of Contents – Volume 20, Number 8—August 2014
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Manoj Murhekar, National Institute of Epidemiology, Indian Council of Medical Research, Chennai-600 070, India
Top