Volume 23, Number 1—January 2017
Research
Estimated Incidence of Antimicrobial Drug–Resistant Nontyphoidal Salmonella Infections, United States, 2004–2012
Figure 3
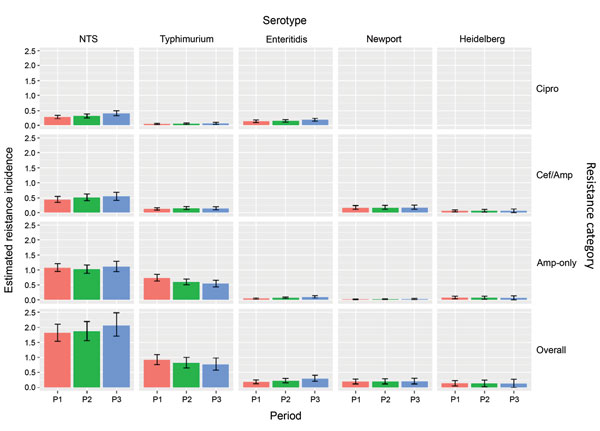
Figure 3. Estimated incidence of NTS infections with clinically important resistance (no. infections/100,000 person-years), by period, serotype, and resistance category, United States, 2004–2012. Estimates were derived by using Bayesian hierarchical models. All NTS includes the 4 major and other serotypes. Three mutually exclusive resistance categories were defined. Isolates in each category may have resistance to other agents. Data on Cipro among Newport (8 isolates), Cipro among Heidelberg (7), and Cef/Amp among Enteritidis (2) were too sparse to use in the Bayesian hierarchical models. Overall resistance was defined as Cipro, Cef/Amp, or Amp-only. Data were grouped into 3 periods (P): 2004–2006 (P1), 2007–2009 (P2), and 2010–2012 (P3). Error bars indicate 95% credible intervals. Amp-only, resistant to ampicillin (MIC >32 μg/mL) but susceptible to ceftriaxone and ciprofloxacin; Cef/Amp, resistant to ceftriaxone (MIC >4 μg/mL) and ampicillin; Cipro, nonsusceptible to ciprofloxacin (MIC >0.12 μg /mL) but susceptible to ceftriaxone; NTS, nontyphoidal Salmonella; P, period.
References
- Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011;17:7–15. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. 2013 [cited 2016 May 10]. http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf
- Gould LH, Walsh KA, Vieira AR, Herman K, Williams IT, Hall AJ, et al.; Centers for Disease Control and Prevention. Surveillance for foodborne disease outbreaks - United States, 1998-2008. MMWR Surveill Summ. 2013;62:1–34.PubMedGoogle Scholar
- Centers for Disease Control and Prevention (CDC). Surveillance for foodborne disease outbreaks—United States, 2009-2010. MMWR Morb Mortal Wkly Rep. 2013;62:41–7.PubMedGoogle Scholar
- Varma JK, Greene KD, Ovitt J, Barrett TJ, Medalla F, Angulo FJ. Hospitalization and antimicrobial resistance in Salmonella outbreaks, 1984-2002. Emerg Infect Dis. 2005;11:943–6. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. National Enteric Disease Surveillance: Salmonella annual report, 2012 [cited 2016 May 10]. http://wwwdev.cdc.gov/ncezid/dfwed/pdfs/salmonella-annual-report-2012-508c.pdf
- Crim SM, Griffin PM, Tauxe R, Marder EP, Gilliss D, Cronquist AB, et al.; Centers for Disease Control and Prevention (CDC). Preliminary incidence and trends of infection with pathogens transmitted commonly through food - Foodborne Diseases Active Surveillance Network, 10 U.S. sites, 2006-2014. MMWR Morb Mortal Wkly Rep. 2015;64:495–9.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS): human isolates final report, 2013. Atlanta: The Centers; 2015.
- Medalla F, Hoekstra RM, Whichard JM, Barzilay EJ, Chiller TM, Joyce K, et al. Increase in resistance to ceftriaxone and nonsusceptibility to ciprofloxacin and decrease in multidrug resistance among Salmonella strains, United States, 1996-2009. Foodborne Pathog Dis. 2013;10:302–9. DOIPubMedGoogle Scholar
- McDermott PF. Antimicrobial resistance in nontyphoidal salmonellae. In: Aarestrup FM, editor. Antimicrobial resistance in bacteria of animal origin. Washington (DC): ASM Press; 2006. p. 293–314.
- Jones TF, Ingram LA, Cieslak PR, Vugia DJ, Tobin-D’Angelo M, Hurd S, et al. Salmonellosis outcomes differ substantially by serotype. J Infect Dis. 2008;198:109–14. DOIPubMedGoogle Scholar
- Pegues DA, Miller SI. Salmonella species. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Philadelphia (PA): Elsevier/Saunders, 2015. p. 2559–68.
- Crump JA, Barrett TJ, Nelson JT, Angulo FJ. Reevaluating fluoroquinolone breakpoints for Salmonella enterica serotype Typhi and for non-Typhi salmonellae. Clin Infect Dis. 2003;37:75–81. DOIPubMedGoogle Scholar
- Gupta A, Fontana J, Crowe C, Bolstorff B, Stout A, Van Duyne S, et al.; National Antimicrobial Resistance Monitoring System PulseNet Working Group. Emergence of multidrug-resistant Salmonella enterica serotype Newport infections resistant to expanded-spectrum cephalosporins in the United States. J Infect Dis. 2003;188:1707–16. DOIPubMedGoogle Scholar
- Fisk TL, Lundberg BE, Guest JL, Ray S, Barrett TJ, Holland B, et al. Invasive infection with multidrug-resistant Salmonella enterica serotype typhimurium definitive type 104 among HIV-infected adults. Clin Infect Dis. 2005;40:1016–21. DOIPubMedGoogle Scholar
- Helms M, Simonsen J, Mølbak K. Quinolone resistance is associated with increased risk of invasive illness or death during infection with Salmonella serotype Typhimurium. J Infect Dis. 2004;190:1652–4. DOIPubMedGoogle Scholar
- Krueger AL, Greene SA, Barzilay EJ, Henao O, Vugia D, Hanna S, et al. Clinical outcomes of nalidixic acid, ceftriaxone, and multidrug-resistant nontyphoidal salmonella infections compared with pansusceptible infections in FoodNet sites, 2006-2008. Foodborne Pathog Dis. 2014;11:335–41. DOIPubMedGoogle Scholar
- Varma JK, Molbak K, Barrett TJ, Beebe JL, Jones TF, Rabatsky-Ehr T, et al. Antimicrobial-resistant nontyphoidal Salmonella is associated with excess bloodstream infections and hospitalizations. J Infect Dis. 2005;191:554–61. DOIPubMedGoogle Scholar
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-fifth informational supplement (M100–S25). Wayne (PA): The Institute; 2015.
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput. 2000;10:325–37. DOIGoogle Scholar
- US Census Bureau. Population estimates [cited 2016 May 10]. http://www.census.gov/popest/
- Ghosh M, Rao JNK. Small area estimation: an appraisal. Stat Sci. 1994;9:5576.
- Sturtz S, Ligges U, Gelman A. R2WinBUGS: a package for running WinBUGS from R. J Stat Softw. 2005;12:1–16. DOIGoogle Scholar
- Lambert PC, Sutton AJ, Burton PR, Abrams KR, Jones DR. How vague is vague? A simulation study of the impact of the use of vague prior distributions in MCMC using WinBUGS. Stat Med. 2005;24:2401–28. DOIPubMedGoogle Scholar
- Crump JA, Medalla FM, Joyce KW, Krueger AL, Hoekstra RM, Whichard JM, et al.; Emerging Infections Program NARMS Working Group. Antimicrobial resistance among invasive nontyphoidal Salmonella enterica isolates in the United States: National Antimicrobial Resistance Monitoring System, 1996 to 2007. Antimicrob Agents Chemother. 2011;55:1148–54. DOIPubMedGoogle Scholar
- Boore AL, Hoekstra RM, Iwamoto M, Fields PI, Bishop RD, Swerdlow DL. Salmonella enterica infections in the United States and assessment of coefficients of variation: a novel approach to identify epidemiologic characteristics of individual serotypes, 1996–2011. PLoS One. 2015;10:e0145416. DOIPubMedGoogle Scholar
- Greene SK, Stuart AM, Medalla FM, Whichard JM, Hoekstra RM, Chiller TM. Distribution of multidrug-resistant human isolates of MDR-ACSSuT Salmonella Typhimurium and MDR-AmpC Salmonella Newport in the United States, 2003-2005. Foodborne Pathog Dis. 2008;5:669–80. DOIPubMedGoogle Scholar
- Iwamoto M, Huang JY, Cronquist AB, Medus C, Hurd S, Zansky S, et al.; Centers for Disease Control and Prevention (CDC). Bacterial enteric infections detected by culture-independent diagnostic tests—FoodNet, United States, 2012-2014. MMWR Morb Mortal Wkly Rep. 2015;64:252–7.PubMedGoogle Scholar
- Angulo FJ, Nargund VN, Chiller TC. Evidence of an association between use of anti-microbial agents in food animals and anti-microbial resistance among bacteria isolated from humans and the human health consequences of such resistance. J Vet Med B Infect Dis Vet Public Health. 2004;51:374–9. DOIPubMedGoogle Scholar
- Dutil L, Irwin R, Finley R, Ng LK, Avery B, Boerlin P, et al. Ceftiofur resistance in Salmonella enterica serovar Heidelberg from chicken meat and humans, Canada. Emerg Infect Dis. 2010;16:48–54. DOIPubMedGoogle Scholar
- Folster JP, Pecic G, Singh A, Duval B, Rickert R, Ayers S, et al. Characterization of extended-spectrum cephalosporin-resistant Salmonella enterica serovar Heidelberg isolated from food animals, retail meat, and humans in the United States 2009. Foodborne Pathog Dis. 2012;9:638–45. DOIPubMedGoogle Scholar
- US Food and Drug Administration. Guidance for industry: the judicious use of medically important antimicrobial drugs in food-producing animals. #209. 2012 [cited 2016 May 10]. http://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/GuidanceforIndustry/UCM216936.pdf
- Cogliani C, Goossens H, Greko C. Restricting antimicrobial use in food animals: lessons from Europe. Microbe. 2011;6:274–9.
- Dechet AM, Scallan E, Gensheimer K, Hoekstra R, Gunderman-King J, Lockett J, et al.; Multistate Working Group. Outbreak of multidrug-resistant Salmonella enterica serotype Typhimurium Definitive Type 104 infection linked to commercial ground beef, northeastern United States, 2003-2004. Clin Infect Dis. 2006;42:747–52. DOIPubMedGoogle Scholar
- Varma JK, Marcus R, Stenzel SA, Hanna SS, Gettner S, Anderson BJ, et al. Highly resistant Salmonella Newport-MDRAmpC transmitted through the domestic US food supply: a FoodNet case-control study of sporadic Salmonella Newport infections, 2002-2003. J Infect Dis. 2006;194:222–30. DOIPubMedGoogle Scholar
- O’Donnell AT, Vieira AR, Huang JY, Whichard J, Cole D, Karp BE. Quinolone-resistant Salmonella enterica serotype Enteritidis infections associated with international travel. Clin Infect Dis. 2014;59:e139–41. DOIPubMedGoogle Scholar
- McDonough PL, Fogelman D, Shin SJ, Brunner MA, Lein DH. Salmonella enterica serotype Dublin infection: an emerging infectious disease for the northeastern United States. J Clin Microbiol. 1999;37:2418–27.PubMedGoogle Scholar
- The White House, Office of the Press Secretary. Executive order—combating antibiotic-resistant bacteria. 2014 [cited 2016 Aug 31]. https://www.whitehouse.gov/the-press-office/2014/09/18/executive-order-combating-antibiotic-resistant-bacteria
- The White House. National strategy for combating antibiotic-resistant bacteria. 2014 [cited 2016 Aug 31]. https://www.whitehouse.gov/sites/default/files/docs/carb_national_strategy.pdf