Volume 26, Number 11—November 2020
Research
Endotheliopathy and Platelet Dysfunction as Hallmarks of Fatal Lassa Fever
Figure 3
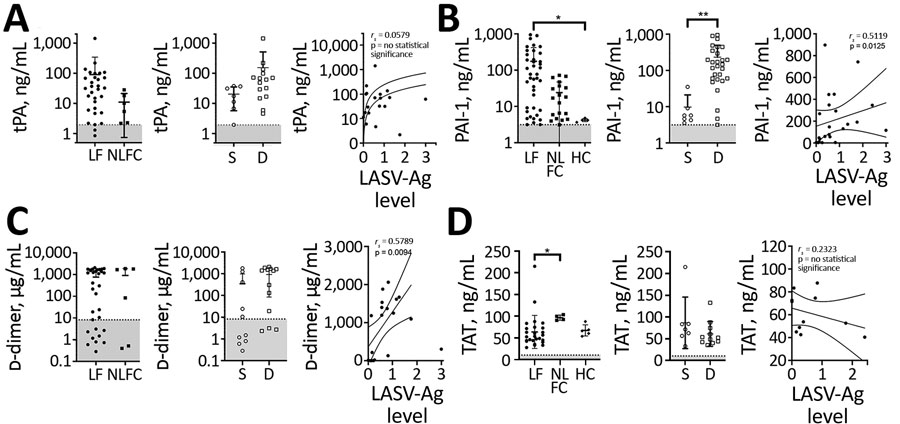
Figure 3. Laboratory findings for fibrinolysis markers for patients with acute LF, NLFCs, and healthy controls HCs, Sierra Leone, 2015–2018. A) Levels of tPA were not statistically significantly different between groups (Kruskal-Wallis p = 0.0516); no differences in tPA were observed between LF (n = 31) and NLFC (n = 6), or between patients who survived (n = 7) and patients who died (n = 15). B) PAI-1 levels predict fatal outcomes (Kruskal-Wallis p<0.0001 across all groups); PAI-1 was statistically significantly elevated (*p = 0.0145) in patients with acute LF (n = 40) compared with HCs (n = 5); patients who died (n = 28) had higher levels of PAI-1 (**p = 0.0031) than those who survived (n = 7); statistically significant positive correlation was observed between PAI-1 and LASV antigen in LF patients (n = 23). C) D-dimer levels in plasma were not statistically significantly different between groups (Kruskal-Wallis p = 0.2167); no difference in D-dimer levels were observed between LF (n = 32) and NLFC (n = 6), nor between patients who died (n = 13) and those who survived (n = 10); and a statistically significant positive correlation was observed between D-dimer levels and LASV antigen in LF patients (n = 19). D) No increased levels of TAT were observed between LF (n = 26) and HC (n = 5) (*p value), nor between patients who survived (n = 7) and died (n = 11), and no statistically significant correlation was observed between TAT levels and LASV-Ag in LF patients (n = 11). Limits of detection are indicated by dashed lines and gray shading below. Error bars show SDs; horizontal lines indicate means. D, died; HC, healthy control; LF, Lassa fever; LASV-Ag, Lassa fever virus antigen; NLFC, non-LF febrile control; PAI-1, plasminogen activator inhibitor 1; S, survived; TAT, thrombinantithrombin complexes; THBD, thrombomodulin; tPA, tissue plasminogen activator.
1These authors contributed equally to this article.