Volume 26, Number 11—November 2020
Dispatch
KPC-3–Producing Serratia marcescens Outbreak between Acute and Long-Term Care Facilities, Florida, USA
Abstract
We describe an outbreak caused by Serratia marcescens carrying blaKPC-3 that was sourced to a long-term care facility in Florida, USA. Whole-genome sequencing and plasmid profiling showed involvement of 3 clonal lineages of S. marcescens and 2 blaKPC-3-carrying plasmids. Determining the resistance mechanism is critical for timely implementation of infection control measures.
Serratia marcescens has been linked to healthcare-associated outbreaks, particularly after use of colistin, which is intrinsically resistant to polymyxins (1,2). Outbreaks of carbapenemase-producing Enterobacteriaceae (CPE) in long-term care facilities (LTCF) have been well described (3,4); outbreaks of the closely related carbapenemase-producing (CP)–S. marcescens are unusual. We describe an outbreak in 2 hospitals in Florida, USA, of S. marcescens producing Klebsiella pneumoniae carbapenemase (KPC). Subsequent investigation identified a local LTCF as the source.
In June 2018, a 382-bed hospital that is part of a large hospital health system network in Miami, Florida, identified an increase of CP–S. marcescens. A retrospective search for more cases included all patients admitted to any facility in the 4-hospital network during October 2017–June 2018 using the automatic surveillance system (VigiLanz; VigiLanz Corporation, https://vigilanzcorp.com) with interface to the electronic medical record (EMR).
We defined cases as patients with carbapenem-resistant S. marcescens by Clinical and Laboratory Standards Institute (CLSI) breakpoints (5) isolated from any source, including clinical or surveillance cultures, during October 2017–December 2018. Based on Centers for Disease Control and Prevention guidelines, community-onset events (CO) were those cases identified <3 days after hospital admission; hospital-onset (HO) were those for which the specimens were collected >4 days after hospital admission (6).
In response to the outbreak, and in addition to interventions in place to prevent hospital-acquired infections (Appendix Table 1), all possible cases were prospectively identified upon admission to any of the network facilities via automatic surveillance system. Transfer forms and regular communication with the local Department of Health (DOH) notified hospitals when a known case-patient was transferred from the LTCF. All patients admitted from the source LTCF were placed in contact precautions at admission and screened for CPE. If positive, patients were placed in enhanced contact precautions (Appendix Table 1) for the duration of their stay. Miami-Dade DOH provided infection prevention and control education and support to the LTCF.
We performed matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry (bioMérieux, https://www.biomerieux-diagnostics.com) and Biofire BCID panel (bioMérieux) for bacterial identification. We conducted susceptibility testing using Vitek2 (bioMérieux) following CLSI guidelines. We tested carbapenemase production with CarbaNP test (Hardy Diagnostics, https://hardydiagnostics.com). We processed active surveillance testing (AST) using a 10 μg meropenem disk on MacConkey plate after broth enrichment; possible CPE colonies were identified and tested for carbapenemase production.
We subjected 1 isolate per patient to whole-genome sequencing on NextSeq500 (Illumina, https://www.illumina.com). We assembled sequences by SPAdes version 3.13 (https://github.com/ablab/spades) and annotated them by prokka version 1.14 (https://github.com/tseemann/prokka). Snippy version 4.4.0 (https://github.com/tseemann/snippy) was used to identify SNPs. We used ResFinder 3.2 (https://cge.cbs.dtu.dk/services/ResFinder) and PlasmidFinder 2.0 (https://cge.cbs.dtu.dk/services/PlasmidFinder) to identify antimicrobial resistance genes and plasmid replicons. We generated a SNP phylogenetic tree with RAxMLversion 8.2.11 (https://github.com/stamatak/standard-RAxML) and visualized it using Interactive Tree of Life (iTOL) version 5 (https://itol.embl.de) (7). We sequenced isolates 505 and 514 using the MinION platform (Oxford Science Park, UK, https://nanoporetech.com/products/minion) to define the blaKPC-harboring plasmids. We used Unicycler version 0.4.8-β (https://github.com/rrwick/Unicycler) for hybrid assembly of Illumina and MinION reads; we confirmed the presence of identified plasmids by aligning Illumina reads to the identified plasmid sequences.
We purified plasmids by alkaline-lysis method and used them to transform Escherichia coli TOP10 by electroporation (8). We selected transformants harboring blaKPC-3 on lysogenic agar with ampicillin, and confirmed acquisition of plasmids by PCR. The plasmids were extracted from the E. coli transformants, digested (EcoRI or HindIII), and run on 0.7% gel to obtain restriction patterns.
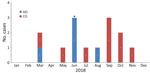
During October 2017–December 2018, a total of 14 patients with CP–S. marcescens were identified in our hospitals (Figure 1); all patients resided at a neighboring LTCF (Table 1). Five cases (36%) were HO, but 4 were detected <15 days after admission and did not coincide in location or time with the other cases. Transmission within the hospital was not suspected; those patients were possibly colonized at admission but undetected due to low sensitivity of AST protocols. The fifth patient had long length-of-stay and previous bloodstream infection (BSI) with KPC-producing Klebsiella pneumoniae.
Ten patients had >1 rectal AST; all were negative. Twelve patients had >1 tracheal aspirate AST; 2 were positive for CP–S. marcescens (susceptibilities in Table 2; Appendix Table 2). Ten cases had clinical infections by CP–S. marcescens including pneumonia (n = 9) and bloodstream infection (n = 4). Most cases were treated empirically with piperacillin/tazobactam, cefepime, and vancomycin. Targeted treatments included ceftazidime/avibactam. Four cases were colonized without signs or symptoms of CP-S. marcescens infection during hospital admission. Three patients died (21% in-hospital mortality); these deaths were not associated with infection by CP-S.marcescens.
During June 2018–January 2019, the 67 notifications of admissions from the source LTCF were related to 30 individual patients. In 7 cases (23%), CP–S. marcescens was present at admission.
We performed molecular testing on 12 isolates, 1 per patient. Core genome analysis demonstrated the presence of 3 clonal lineages of blaKPC-3-carrying S. marcescens involving >1 patient, and 1 outlier (Figure 2). Eleven isolates belonging to the 3 lineages shared a 43-kb FII-type blaKPC-3-harboring plasmid, which had >99% sequence identity with pKPC_Kp46 plasmid previously described in K. pneumoniae (GenBank accession no. KX348146.1) (9); confirmation was by an identical plasmid restriction profile. Lineage 1 isolates shared a 19-kb ColRNAI-type blaKPC-3-harboring plasmid, 99% identical to previously reported pNJST258C2 from K. pneumoniae (GenBank accession no. CP006919.1), except for the absence of the transposable element containing aminoglycoside resistance genes aacA1 and aacA4 (10). The outlying isolate, 520, only contained a pNJST258C2-like blaKPC-3-harboring plasmid identical to that found in lineage 1. The blaKPC-3 sequence was identical between the 2 plasmids and was located on Tn4401b-like elements, which were identical except for a 70-bp deletion in tnpA leading to frameshift and premature stop in the pNJST258C2-like plasmid. This deletion did not seem to affect KPC expression; isolate 520, carrying only the pNJST258C2-like plasmid, was still resistant to carbapenems. In addition to blaKPC-3, the pKPC_Kp46–like plasmid contained blaTEM-1, ΔblaOXA-9, and qnrB19. The pNJST258C2-like plasmid did not contain additional antimicrobial resistance genes; however, it contained an operon encoding production of colicin, an antimicrobial substance that is lethal against related strains that lack it (11). Isolate 520 was from the patient with a history of KPC-producing K. pneumoniae, suggesting that the blaKPC-3-harboring plasmid was transferred to S. marcescens in the patient in a separate event from the infection of the other 11 cases.
Use of an automatic surveillance system enabled retrospective and prospective detection of cases and identification of their common exposure in an LTCF on the basis of shared address. Prospective identification of residents of the source LTCF enabled screening at point of entry and implementation of interventions to prevent hospital transmission. Direct communication between the infection control department and the LTCF was difficult and relied upon the local DOH to share information about known cases. Unfortunately, a regional registry of patients with CPE is not available in Florida (12,13).
The pKPC-KP4–like plasmid shared among the 3 clonal lineages involved in the outbreak, and the pNJST258C2-like plasmid, shared between lineage 1 and the outlier isolate, were the vehicles of blaKPC-3 in this polyclonal outbreak. However, it is unclear why lineage 1 isolates contained both blaKPC-3-harboring plasmids. It is possible that in addition to antimicrobial resistance, factors such as colicin production facilitated dissemination within the LTCF.
In summary, our investigation of this CP–S. marcescens outbreak in 2 hospitals in Florida identified a local LTCF as the source. Early identification, communication, and implementation of preventive measures within healthcare facilities and cooperation with local public health authorities are pivotal in preventing transmission of multidrug-resistant organisms among vulnerable populations.
Ms. Jimenez is an infection preventionist at Jackson Health System in Miami, Florida, and a doctoral candidate at Robert Stempel School of Social Work and Public Health, Epidemiology Department of Florida International University in Miami, Florida. Her primary research interest is the epidemiology of multidrug-resistant bacilli and the prevention of hospital-acquired infections.
Acknowledgments
We thank Daniel R. Evans for his assistance with MinION sequencing and Marissa P. Griffith for bioinformatics support.
A.I. was supported through Physician Scientist Incubator Program at the University of Pittsburgh, sponsored by the Burrows Wellcome Fund. Y.D. was supported by research grants from the National Institutes of Health (grant nos. R01AI104895, R21AI135522, and R21AI151362).
References
- Gaynes R, Edwards JR, Edwards JR, Edwards JR; National Nosocomial Infections Surveillance System. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005;41:848–54. DOIPubMedGoogle Scholar
- Merkier AK, Rodríguez MC, Togneri A, Brengi S, Osuna C, Pichel M, et al.; Serratia marcescens Argentinean Collaborative Group. Outbreak of a cluster with epidemic behavior due to Serratia marcescens after colistin administration in a hospital setting. J Clin Microbiol. 2013;51:2295–302. DOIPubMedGoogle Scholar
- Legeay C, Hue R, Berton C, Cormier H, Chenouard R, Corvec S, et al. Control strategy for carbapenemase-producing Enterobacteriaceae in nursing homes: perspectives inspired from three outbreaks. J Hosp Infect. 2019;101:183–7. DOIPubMedGoogle Scholar
- Kelly AM, Mathema B, Larson EL. Carbapenem-resistant Enterobacteriaceae in the community: a scoping review. Int J Antimicrob Agents. 2017;50:127–34. DOIPubMedGoogle Scholar
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, 28th edition (supplement M100). Wayne (PA): The Institute; 2018.
- Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) patient safety component manual. 2018 January [cited 2020 Sep 28]. https://www.cdc.gov/nhsn/pdfs/validation/2018/pcsmanual_2018-508.pdf
- Letunic I, Bork P. Interactive Tree Of Life (iTOL) v4: recent updates and new developments. Nucleic Acids Res. 2019;47(W1):W256–9. DOIPubMedGoogle Scholar
- Sidjabat HE, Paterson DL, Qureshi ZA, Adams-Haduch JM, O’Keefe A, Pascual A, et al. Clinical features and molecular epidemiology of CMY-type β-lactamase-producing Escherichia coli. Clin Infect Dis. 2009;48:739–44. DOIPubMedGoogle Scholar
- Kim JO, Song SA, Yoon EJ, Shin JH, Lee H, Jeong SH, et al. Outbreak of KPC-2-producing Enterobacteriaceae caused by clonal dissemination of Klebsiella pneumoniae ST307 carrying an IncX3-type plasmid harboring a truncated Tn4401a. Diagn Microbiol Infect Dis. 2017;87:343–8. DOIPubMedGoogle Scholar
- Deleo FR, Chen L, Porcella SF, Martens CA, Kobayashi SD, Porter AR, et al. Molecular dissection of the evolution of carbapenem-resistant multilocus sequence type 258 Klebsiella pneumoniae. Proc Natl Acad Sci U S A. 2014;111:4988–93. DOIPubMedGoogle Scholar
- Cascales E, Buchanan SK, Duché D, Kleanthous C, Lloubès R, Postle K, et al. Colicin biology. Microbiol Mol Biol Rev. 2007;71:158–229. DOIPubMedGoogle Scholar
- Clarivet B, Pantel A, Morvan M, Jean Pierre H, Parer S, Jumas-Bilak E, et al. Carbapenemase-producing Enterobacteriaceae: use of a dynamic registry of cases and contacts for outbreak management. J Hosp Infect. 2016;92:73–7. DOIPubMedGoogle Scholar
- Lee BY, Bartsch SM, Hayden MK, Welling J, DePasse JV, Kemble SK, et al. How introducing a registry with automated alerts for carbapenem-resistant Enterobacteriaceae (CRE) may help control CRE spread in a region. Clin Infect Dis. 2020;70:843–9.PubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: October 14, 2020
Table of Contents – Volume 26, Number 11—November 2020
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Adriana Jimenez, Department of Infection Prevention and Control, Jackson Health System, 1611 NW 12th Ave, Park Plaza West L-301, Miami, FL 33136, USA
Top