Volume 26, Number 5—May 2020
Dispatch
Species Distribution and Isolation Frequency of Nontuberculous Mycobacteria, Uruguay
Abstract
Nontuberculous mycobacteria (NTM) increasingly are recognized as opportunistic pathogens of humans. NTM species distribution is well documented in Europe and North America, but data from other regions are scarce. We assessed NTM isolation frequency and species distribution in Uruguay during 2006–2018.
Nontuberculous mycobacteria (NTM) are comprised of >150 species (1) and are increasingly recognized as opportunistic pathogens (2). In addition, frequency of disease-causing NTM isolation has been rising in many settings (3,4). The exact epidemiology of NTM pulmonary disease, the most common manifestation in adults (3), has been difficult to determine because reporting is not mandatory in most countries and identification of true disease is often difficult (5).
The distribution of NTM species isolated from human clinical samples varies greatly by region (6). In South America, data on NTM isolation frequencies are available for São Paulo and Rio de Janeiro, Brazil (7–9) and Buenos Aires, Argentina (6). Because clinical and laboratory observations suggested an emergence of NTM isolates, we conducted a retrospective study of isolation frequency of NTM in Uruguay.
We conducted a retrospective study of data on all NTM isolates identified at the Comisión Honoraria de Lucha Anti-Tuberculosis (Montevideo, Uruguay), the national tuberculosis reference laboratory, during January 2006–December 2018. The laboratory receives samples from all suspected tuberculosis (TB) cases across the country and performs universal acid-fast bacillus smear testing and solid culture in Löwenstein-Jensen and Ogawa egg-based media as a part of routine diagnostic testing. We abstracted basic patient demographic information and NTM identification results from the laboratory databases.
Phenotypic characterization of isolated NTM was performed by using biochemical methods, and complementary genotyping identification was introduced in 2012 by using GenoType Mycobacterium CM (Hain Lifescience GmbH, https://www.hain-lifescience.de). In 2016, the laboratory included GenoType Mycobacterium AS (Hain Lifescience GmbH) in its pipeline and retrospectively identified previously unidentified isolates.
For comparison, we also collected data on the number of culture-positive TB cases during the study period from the laboratory databases. We used official population information from the National Institute of Statistics Uruguay (Instituto Nacional de Estadística, http://www.ine.gub.uy) to calculate NTM incidence (Appendix 1).
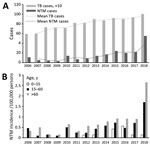
During 2006–2018, a total of 255 NTM isolates were collected from pulmonary and extrapulmonary samples from 204 patients, 143 male and 61 female, in Uruguay (Table 1). Most (147/255; 57.6%) isolates identified were members of the Mycobacterium avium complex (MAC), which includes M. intracellulare and M. avium; 21 (8.2%) were M. kansasii; 15 were M. gordonae (5.9%); and 12 were M. peregrinum (4.7%) (Table 2). We observed an increase in NTM isolation frequency and an increase in TB cases during 2011–2018 (Figure 1, panel A). We also calculated an age-adjusted isolation frequency to determine population aging effect (Figure 1, panel B).
Among 204 cases, 23 patients had >1 NTM-positive isolate 6 months apart, and 13 had positive cultures for >2 years. Patients >50 years of age (mean 52 years of age) were more likely to have prolonged culture-positivity, a statistically significant difference from patients with a single positive culture (mean 42.6 years of age; p = 0.0099). Most (7/13; 53.8%) prolonged infections were caused by M. intracellulare, and 4 prolonged cases remained NTM-positive for <6 years, including 2 infections with M. intracellulare and 1 each with M. kansasii and M. heckeshornense. Most (10/13; 76.9%) prolonged cases were detected in pulmonary isolates.
Only 4 (1.9%) cases showed disseminated infections in isolates obtained from hemoculture, bone marrow culture, ganglion biopsy, feces, urine, or sputum of the same patient. Among the 4 disseminated infections, M. avium was isolated from 2 cases, M. genavense from 1 case, and M. intracellulare from 1 case.
The incidence of NTM in Uruguay increased from 0.33 cases/100,000 inhabitants in 2006 to 1.57 cases/100,000 inhabitants to 2018 (Figure 1, panel A). In 2018, the incidence of NTM was 2.73/100,000 inhabitants in the north, which has only 16.72% of the total population of the country. In the south, where 83.28% of the population lives, the incidence was much lower, 1.34 cases/100,000 inhabitants. Culture-positive TB cases showed a reverse tendency with statistically significant differences. The incidence rate for TB was higher in the south, 30.01 cases/100,000 inhabitants, and lower in the north, 21.50 cases/100,000 inhabitants (Figure 2).
During the period studied, we observed a 4-fold increase in the NTM isolation rate (Appendix 1). Implementation of new detection techniques during this timeframe could account for part of the increase (10). However, we noted a >2-fold increase (2.49) in number of isolates recorded during 2017–2018, when no laboratory protocol changes were introduced, suggesting the NTM incidence is rising in Uruguay (Appendix 1).
Rivero-Lezcano et al. (10) suggested changes in the pathogen and an aging population could explain the rising incidence of NTM isolation and disease. From 2017 to 2018, we observed a higher increase in NTM incidence (2.94 cases/100,000 persons) among persons >60 years of age compared with persons 15–60 years of age (2.39 cases/100,000 persons) (Figure 1, panel B). However, we noted that the age composition of the population remained stable over time (Appendix 1), suggesting other factors are driving increases in NTM isolation rates.
MAC is reported to be the most frequently isolated NTM species in all continents (3), but we observed a different species distribution than previously reported for South America. We saw a higher prevalence of M. intracellulare (33.7% of isolates) than M. avium (23.9% of isolates) (Table 2). We found species not previously reported in Latin America, including M. xenopi and M. arupense, and M. malmoense, which typically is found in northern Europe (11). We also found M. parakoreense, for which only 2 cases are reported in the literature, 1 case in 2013 isolated from a single clinical sample (12) and another in Africa (13). In addition, we noted 2 cases of M. heckeshornense, a species previously reported by our group (14).
We noted prolonged positivity in 6% (13/204) of NTM cases. MAC was responsible for most (69%) prolonged culture positives and M. kansasii was responsible for 15% of prolonged positivity.
We believe the differences observed in NTM isolation rates between regions of Uruguay could be explained by climate factors. The higher temperatures and increased rainfall in the north could favor the incidence ambient pathogens (Appendix 2). We also cannot disregard differences associated with other factors, such as the age of the population.
Our study has several limitations. First, the public health system of Uruguay only registers M. tuberculosis; clinical data of NTM patients are difficult to obtain. In addition, the GenoType AS assay used to identify NTM does not detect all NTM species; including genomic sequencing-based identification methods would improve detection in the future. Identification of NTM species is crucial for determining appropriate clinical and antimicrobial treatment for pulmonary NTM, which are dependent on the characteristics of the species (8).
Our findings indicate that rate of NTM have risen nearly 5-fold (4.79) in Uruguay, from 0.33 cases/100,000 inhabitants in 2006 to 1.57 cases/100,000 inhabitants in 2018. The species distribution largely aligns with existing data from elsewhere in South America, which demonstrates a predominance of MAC. Prolonged culture positivity and various isolation sites sources suggest that NTM disease is prevalent in Uruguay and warrants further studies to optimize diagnosis and treatment.
Dr. Greif is a molecular biologist at the Institut Pasteur Montevideo, Montevideo, Uruguay. His research interests include developing molecular methods for diagnosing mycobacteria.
Acknowledgments
We thank Carlos Rivas for his support and efforts to preserve nontuberculous mycobacteria data at the Comisión Honoraria de Lucha Anti-Tuberculosis.
G.G. and C.R. are supported by the Sistema Nacional de Investigadores, Uruguay.
References
- Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27:727–52. DOIPubMedGoogle Scholar
- Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al.; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416. DOIPubMedGoogle Scholar
- Zweijpfenning SMH, Ingen JV, Hoefsloot W. Geographic distribution of nontuberculous mycobacteria isolated from clinical specimens: a systematic review. Semin Respir Crit Care Med. 2018;39:336–42. DOIPubMedGoogle Scholar
- Schiff HF, Jones S, Achaiah A, Pereira A, Stait G, Green B. Clinical relevance of non-tuberculous mycobacteria isolated from respiratory specimens: seven year experience in a UK hospital. Sci Rep. 2019;9:1730. DOIPubMedGoogle Scholar
- Prevots DR, Loddenkemper R, Sotgiu G, Migliori GB. Nontuberculous mycobacterial pulmonary disease: an increasing burden with substantial costs. Eur Respir J. 2017;49:
1700374 . DOIPubMedGoogle Scholar - Hoefsloot W, van Ingen J, Andrejak C, Ängeby K, Bauriaud R, Bemer P, et al.; Nontuberculous Mycobacteria Network European Trials Group. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J. 2013;42:1604–13. DOIPubMedGoogle Scholar
- Bensi EP, Panunto PC, Ramos MC. Incidence of tuberculous and non-tuberculous mycobacteria, differentiated by multiplex PCR, in clinical specimens of a large general hospital. Clinics (São Paulo). 2013;68:179–84. DOIPubMedGoogle Scholar
- Marques LRM, Ferrazoli L, Chimara É. Pulmonary nontuberculous mycobacterial infections: presumptive diagnosis based on the international microbiological criteria adopted in the state of São Paulo, Brazil, 2011-2014. [in Portuguese]. J Bras Pneumol. 2019;45:
e20180278 . DOIPubMedGoogle Scholar - de Mello KGC, Mello FC, Borga L, Rolla V, Duarte RS, Sampaio EP, et al. Clinical and therapeutic features of pulmonary nontuberculous mycobacterial disease, Brazil, 1993-2011. Emerg Infect Dis. 2013;19:393–9.PubMedGoogle Scholar
- Rivero-Lezcano OM, González-Cortés C, Mirsaeidi M. The unexplained increase of nontuberculous mycobacteriosis. Int J Mycobacteriol. 2019;8:1–6. DOIPubMedGoogle Scholar
- Jankovic M, Samarzija M, Sabol I, Jakopovic M, Katalinic Jankovic V, Zmak L, et al. Geographical distribution and clinical relevance of non-tuberculous mycobacteria in Croatia. Int J Tuberc Lung Dis. 2013;17:836–41. DOIPubMedGoogle Scholar
- Kim BJ, Hong SH, Yu HK, Park YG, Jeong J, Lee SH, et al. Mycobacterium parakoreense sp. nov., a slowly growing non-chromogenic species related to Mycobacterium koreense, isolated from a human clinical specimen. Int J Syst Evol Microbiol. 2013;63:2301–8. DOIPubMedGoogle Scholar
- Chin’ombe N, Muzividzi B, Munemo E, Nziramasanga P. Molecular identification of nontuberculous mycobacteria in humans in Zimbabwe using 16S ribosequencing. Open Microbiol J. 2016;10:113–23. DOIPubMedGoogle Scholar
- Coitinho C, Greif G, van Ingen J, Laserra P, Robello C, Rivas C. First case of Mycobacterium heckeshornense cavitary lung disease in the Latin America and Caribbean region. New Microbes New Infect. 2015;9:63–5. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: April 09, 2020
Table of Contents – Volume 26, Number 5—May 2020
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Gonzalo Greif, Laboratorio de Interacción Hospedero-Patógeno, Unidad de Biología Molecular, Institut Pasteur Montevideo, Mataojo 2020, Montevideo, Uruguay
Top