Volume 28, Number 3—March 2022
Synopsis
Association of Healthcare and Aesthetic Procedures with Infections Caused by Nontuberculous Mycobacteria, France, 2012‒2020
Figure 2
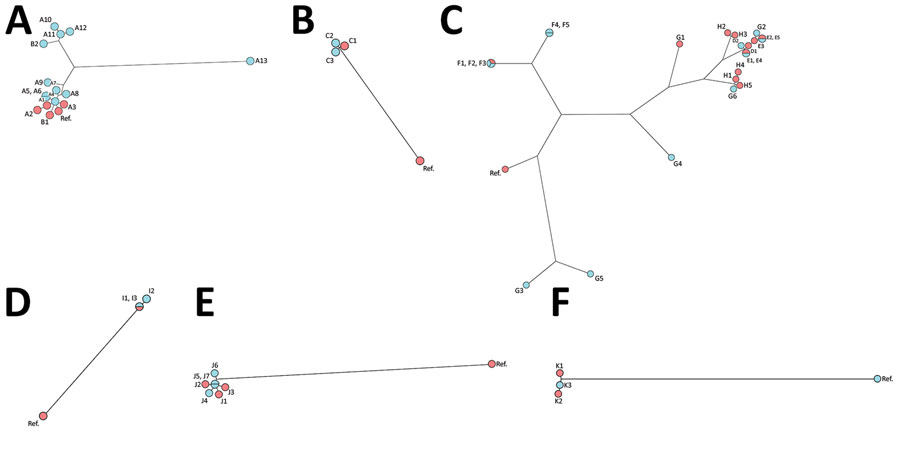
Figure 2. Genomic comparison of nontuberculous mycobacteria isolates by using whole-genome sequencing phylogenetic analysis and maximum parsimony trees. A) Mycobacterium chimaera, B) M. fortuitum, C) M. chelonae, D) M. marinum, E) M. mucogenicum, F) M. neoaurum. Environmental isolates are indicated in blue, and clinical isolates are indicated in red. Additional information for the 6 Mycobacterium species tested is provided in the Appendix. Ref, referent. Panel A: Based on 19,621 single-nucleotide polymorphisms (SNPs) generated from comparison of 16 genomes using square root scaling. Isolates were 1) clinical isolates from 2 patients who had M. chimaera disseminated disease after open-heart surgery (A1 and A2 from the first patient), A3 from the second patient; 2) a reference genome from a previously described epidemic patient (8); 3) 10 heater-cooler unit water samples from the hospital where the second patient underwent surgery, collected 4 years after the report (A4‒A13); 4) clinical sample from a patient who had a breast prosthesis infection (B1); and 5) the environmental isolate collected in the hospital’s water network 1 year after the report of the breast prosthesis infection (B2). Panel B: Based on 27,796 SNPs generated from comparison of 4 genomes using square root scaling. Isolates were 1) clinical isolate from a patient who had M. fortuitum breast prosthesis infection (C1) and 2) environmental isolate collected 1 month after the report in the water supply network in the shower of the patient’s hospital room (C2, C3). Panel C: Based on 67,759 SNPs generated from comparison of 24 genomes using square root scaling. Isolates were 11 clinical isolates: 1 from an infection after face lift surgery (D1), 3 from 2 skin and soft tissue infections after a tattoo (E1‒E2 from the same patient and E3 from another patient who was tattooed in the same tattoo parlor); 2 from 2 mesotherapy infections from 2 nonrelated reports (F1 and G1); and 5 using supply networks were obtained for investigations including: 1 isolate from a surgical sink (D2), 4 isolates from a doctor’s office sink (F2‒F3, G5‒G6), 2 isolates from a tattoo parlor’s sink used to dilute the ink (E4‒E5) and 5 isolates from a patient’s home (F4‒F5, G2‒G4). Panel D: Based on 24,757 SNPs generated from comparison of 4 genomes using square root scaling. Isolates were 1) a clinical isolate from a skin and soft tissue infection caused by contamination after a bath in a balneotherapy swimming pool (I1 and I2) 2 environmental isolates from the swimming pool (I2 and I3). Panel E: Based on 53,551 SNPs generated by comparison of 8 genomes using square root scaling. Isolates were 1) 3 clinical isolates from catheter-associated infections (3 patients J1‒J3) and 2) 4 environmental isolates from hospital water supply networks (J4‒J7). Panel F: Based on 58,473 SNPs generated by comparison of 4 genomes using square root scaling. Isolates were 1) 2 clinical isolates from the blood culture (K1 and K2) of 1 patient and 2) 1 isolate from microbiological control after an autologous stem cell transplant (K3).
References
- Le Dantec C, Duguet JP, Montiel A, Dumoutier N, Dubrou S, Vincent V. Occurrence of mycobacteria in water treatment lines and in water distribution systems. Appl Environ Microbiol. 2002;68:5318–25. DOIPubMedGoogle Scholar
- Falkinham JO III. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015;36:35–41. DOIPubMedGoogle Scholar
- Meyers H, Brown-Elliott BA, Moore D, Curry J, Truong C, Zhang Y, et al. An outbreak of Mycobacterium chelonae infection following liposuction. Clin Infect Dis. 2002;34:1500–7. DOIPubMedGoogle Scholar
- Conaglen PD, Laurenson IF, Sergeant A, Thorn SN, Rayner A, Stevenson J. Systematic review of tattoo-associated skin infection with rapidly growing mycobacteria and public health investigation of a cluster in Scotland, 2010. Euro Surveill. 2013;18:20553. DOIPubMedGoogle Scholar
- Carbonne A, Brossier F, Arnaud I, Bougmiza I, Caumes E, Meningaud JP, et al. Outbreak of nontuberculous mycobacterial subcutaneous infections related to multiple mesotherapy injections. J Clin Microbiol. 2009;47:1961–4. DOIPubMedGoogle Scholar
- Leão SC, Viana-Niero C, Matsumoto CK, Lima KV, Lopes ML, Palaci M, et al. Epidemic of surgical-site infections by a single clone of rapidly growing mycobacteria in Brazil. Future Microbiol. 2010;5:971–80. DOIPubMedGoogle Scholar
- Mora AD, Giraldo S, Castillo DA, Ferro BE. [Clinical behavior of infection and disease caused by non-tuberculous mycobacteria in Latin America: Scoping review] [in Spanish]. Rev Peru Med Exp Salud Publica. 2021;38:318–25. DOIPubMedGoogle Scholar
- van Ingen J, Kohl TA, Kranzer K, Hasse B, Keller PM, Katarzyna Szafrańska A, et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: a molecular epidemiological study. Lancet Infect Dis. 2017;17:1033–41. DOIPubMedGoogle Scholar
- Astagneau P, Desplaces N, Vincent V, Chicheportiche V, Botherel A, Maugat S, et al. Mycobacterium xenopi spinal infections after discovertebral surgery: investigation and screening of a large outbreak. Lancet. 2001;358:747–51. DOIPubMedGoogle Scholar
- Ferry C, Saussine A, Bouaziz JD, Xhaard A, Peffault de Latour R, Ribaud P, et al. Disseminated cutaneous infection due to Mycobacterium chelonae following hematopoietic stem cell transplantation. IDCases. 2014;1:68–9. DOIPubMedGoogle Scholar
- Yuan SM. Mycobacterial endocarditis: a comprehensive review. Rev Bras Cir Cardiovasc. 2015;30:93–103.PubMedGoogle Scholar
- Couderc C, Carbonne A, Thiolet JM, Brossier F, Savey A, Bernet C, et al. [Non-tuberculous mycobacterial infections related to esthetic care in France, 2001-2010] [in French]. Med Mal Infect. 2011;41:379–83. DOIPubMedGoogle Scholar
- Ministry of Social Affairs and Health. Decree no. 2017–129 of February 3, 2017 relating to the prevention of healthcare-associated infections, 2017 [in French] [cited 2021 Dec 9]. https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000033982071
- Rajendran P, Padmapriyadarsini C, Mondal R. Nontuberculous mycobacterium: An emerging pathogen: Indian perspective. Int J Mycobacteriol. 2021;10:217–27.PubMedGoogle Scholar
- European Center for Disease Prevention and Control. Rapid risk assessment: invasive cardiovascular infection by Mycobacterium chimaera potentially associated with heater-cooler units used during cardiac surgery, April 30, 2015 [cited 2021 Jun 28]. https://ecdc.europa.eu/en/publications-data/invasive-cardiovascular-infection-mycobacterium-chimaera-potentially-associated
- Henkle E, Hedberg K, Schafer SD, Winthrop KL. Surveillance of extrapulmonary nontuberculous mycobacteria infections, Oregon, USA, 2007‒2012. Emerg Infect Dis. 2017;23:1627–30. DOIPubMedGoogle Scholar
- Blanc P, Dutronc H, Peuchant O, Dauchy FA, Cazanave C, Neau D, et al. Nontuberculous mycobacterial infections in a French hospital: a 12-year retrospective study. PLoS One. 2016;11:
e0168290 . DOIPubMedGoogle Scholar - Jaubert J, Mougari F, Picot S, Boukerrou M, Barau G, Ali Ahmed SA, et al. A case of postoperative breast infection by Mycobacterium fortuitum associated with the hospital water supply. Am J Infect Control. 2015;43:406–8. DOIPubMedGoogle Scholar
- Regnier S, Cambau E, Meningaud JP, Guihot A, Deforges L, Carbonne A, et al. Clinical management of rapidly growing mycobacterial cutaneous infections in patients after mesotherapy. Clin Infect Dis. 2009;49:1358–64. DOIPubMedGoogle Scholar
- Donohue MJ, Mistry JH, Donohue JM, O’Connell K, King D, Byran J, et al. Increased frequency of nontuberculous mycobacteria detection at potable water taps within the United States. Environ Sci Technol. 2015;49:6127–33. DOIPubMedGoogle Scholar
- Li T, Abebe LS, Cronk R, Bartram J. A systematic review of waterborne infections from nontuberculous mycobacteria in health care facility water systems. Int J Hyg Environ Health. 2017;220:611–20. DOIPubMedGoogle Scholar
- Regnier S, Caumes E. [Non-tuberculous mycobacterial infections related to esthetic care in France, 2001-2010] [in French]. Med Mal Infect. 2011;41:667–8. DOIPubMedGoogle Scholar