Volume 28, Number 4—April 2022
Dispatch
In Vitro Confirmation of Artemisinin Resistance in Plasmodium falciparum from Patient Isolates, Southern Rwanda, 2019
Figure 1
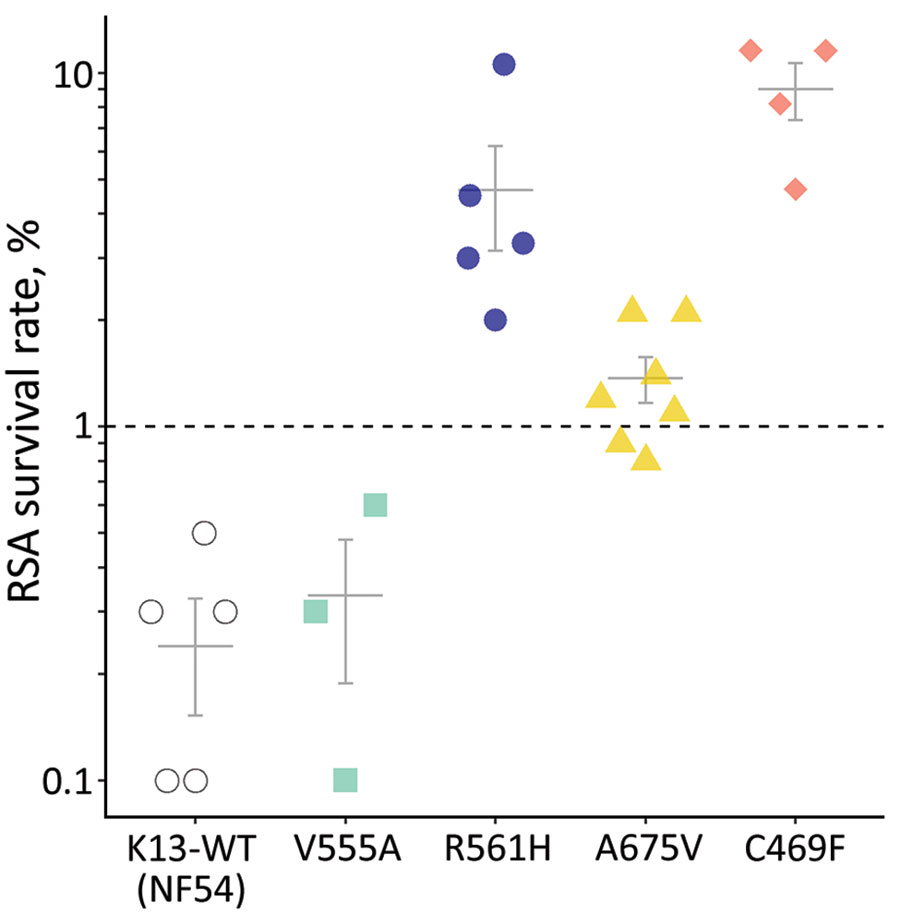
Figure 1. RSA 0–3-hour postinvasion survival rates (%) of an artemisinin-susceptible, K13 WT Plasmodium falciparum strain (NF54) and 4 P. falciparum patient isolates from Rwanda with K13 mutations. Each data point represents the mean of triplicate experiments. Isolate growth rates were only considered for analysis if 72-hour growth rates exceeded 1.5× rates in the nonexposed controls. Indicated error bars display the mean + SE; dashed line indicates the 1% survival rate threshold used to define artemisinin resistance (1,6). K13, kelch 13; RSA, ring-stage susceptibility assay; WT, wild-type.
References
- World Health Organisation Global Malaria Programme. Report on antimalarial drug efficacy, resistance and response: 10 years of surveillance (2010–2019). 2020 [cited 2021 Nov 1]. https://apps.who.int/iris/rest/bitstreams/1316082/retrieve
- Bergmann C, van Loon W, Habarugira F, Tacoli C, Jäger JC, Savelsberg D, et al. Increase in kelch 13 polymorphisms in Plasmodium falciparum, southern Rwanda. Emerg Infect Dis. 2021;27:294–6. DOIPubMedGoogle Scholar
- Uwimana A, Umulisa N, Venkatesan M, Svigel SS, Zhou Z, Munyaneza T, et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect Dis. 2021;21:1120–8. DOIPubMedGoogle Scholar
- Balikagala B, Fukuda N, Ikeda M, Katuro OT, Tachibana SI, Yamauchi M, et al. Evidence of artemisinin-resistant malaria in Africa. N Engl J Med. 2021;385:1163–71. DOIPubMedGoogle Scholar
- Uwimana A, Legrand E, Stokes BH, Ndikumana JM, Warsame M, Umulisa N, et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. [Erratum in: Nat Med. 2021;27:1113–5.]. Nat Med. 2020;26:1602–8. DOIPubMedGoogle Scholar
- Witkowski B, Amaratunga C, Khim N, Sreng S, Chim P, Kim S, et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in-vitro and ex-vivo drug-response studies. Lancet Infect Dis. 2013;13:1043–9. DOIPubMedGoogle Scholar
- Machado M, Murtinheira F, Lobo E, Nogueira F. Whole-cell SYBR Green I assay for antimalarial activity assessment. Ann Clin Med Microbio. 2016;2:1010.
- Preston MD, Campino S, Assefa SA, Echeverry DF, Ocholla H, Amambua-Ngwa A, et al. A barcode of organellar genome polymorphisms identifies the geographic origin of Plasmodium falciparum strains. Nat Commun. 2014;5:4052. DOIPubMedGoogle Scholar
- Hu F, Zou Q, Li Y, Zhu G, Zhou H, Zhang M, et al. A PCR-based technique to track the geographic origin of Plasmodium falciparum with 23-SNP barcode analysis. Front Public Health. 2021;9:
649170 . DOIPubMedGoogle Scholar - Stokes BH, Dhingra SK, Rubiano K, Mok S, Straimer J, Gnädig NF, et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. eLife. 2021;10:
e66277 . DOIPubMedGoogle Scholar - Phyo AP, Ashley EA, Anderson TJC, Bozdech Z, Carrara VI, Sriprawat K, et al. Declining efficacy of artemisinin combination therapy against P. falciparum malaria on the Thai–Myanmar border (2003–2013): the role of parasite genetic factors. Clin Infect Dis. 2016;63:784–91. DOIPubMedGoogle Scholar
- van der Pluijm RW, Imwong M, Chau NH, Hoa NT, Thuy-Nhien NT, Thanh NV, et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect Dis. 2019;19:952–61. DOIPubMedGoogle Scholar
- van Loon W, Bergmann C, Habarugira F, Tacoli C, Savelsberg D, Oliveira R, et al. Changing pattern of Plasmodium falciparum pfmdr1 gene polymorphisms in southern Rwanda. Antimicrob Agents Chemother. 2021;65:
e0090121 . DOIPubMedGoogle Scholar - Veiga MI, Dhingra SK, Henrich PP, Straimer J, Gnädig N, Uhlemann AC, et al. Globally prevalent PfMDR1 mutations modulate Plasmodium falciparum susceptibility to artemisinin-based combination therapies. Nat Commun. 2016;7:11553. DOIPubMedGoogle Scholar
- Tindana P, de Haan F, Amaratunga C, Dhorda M, van der Pluijm RW, Dondorp AM, et al. Deploying triple artemisinin-based combination therapy (TACT) for malaria treatment in Africa: ethical and practical considerations. Malar J. 2021;20:119. DOIPubMedGoogle Scholar
Page created: January 27, 2022
Page updated: March 19, 2022
Page reviewed: March 19, 2022
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.