Volume 29, Number 3—March 2023
Dispatch
Tuberculosis Preventive Therapy among Persons Living with HIV, Uganda, 2016–2022
Abstract
During October 2016–March 2022, Uganda increased tuberculosis (TB) preventive therapy coverage among persons living with HIV from 0.6% to 88.8%. TB notification rates increased from 881.1 to 972.5 per 100,000 persons living with HIV. Timely TB screening, diagnosis, and earlier treatment should remain high priorities for TB/HIV prevention programming.
Tuberculosis (TB) is the leading cause of illness and death globally among persons living with HIV (PLHIV) (1,2). In 2021, among ≈38.4 million PLHIV worldwide, 703,000 TB cases and 187,000 TB-related deaths were reported (3,4). HIV antiretroviral therapy (ART) and TB preventive therapy (TPT) reduce TB incidence and death among PLHIV (5,6). TPT is administered to persons at high risk for TB and who do not have symptoms of active disease; positive tuberculin skin tests or interferon gamma release assays are not required. Although increased ART coverage has coincided with declines in TB-related deaths worldwide, since the early 2000s, TPT scale-up has been limited (3,7,8).
Uganda is a World Health Organization–designated TB and HIV high-burden country (3). By 2020, ≈1,400,000 PLHIV were reported in Uganda; in 2021, a total of 29,000 TB cases and 6,200 TB-related deaths among PLHIV were reported (9,10). In 2015, Uganda accelerated efforts to provide TPT to PLHIV who had no TB symptoms and received support from the US President’s Emergency Plan for AIDS Relief (PEPFAR) (11,12). Further efforts included a 100-day scale-up campaign in 2019, adopting TPT as standard of care for all eligible PLHIV in 2021 (13), and a last-mile campaign launched in June 2022. Therefore, despite the COVID-19 pandemic, TPT scale-up continued. We analyzed data describing TPT scale-up among PLHIV in Uganda and highlight next steps to further reduce TB-related illness and death and reach global targets for treatment coverage.
We sourced semiannual aggregate data during October 2016–March 2022 from the centralized PEPFAR DATIM Monitoring, Evaluation, and Reporting database (Uganda DATIM version 1.31 MER 2.5, updated January 4, 2021; https://ug.datim4u.org). We analyzed trends among PLHIV receiving PEPFAR-supported ART across 5 areas: TPT initiation, defined as beginning any TPT regimen, such as 6-month daily isoniazid or 3-month 1 time/week isoniazid plus rifapentine; TPT completion, defined as receiving a full course of TPT according to data capture tools; TPT completion rates, calculated as the number of TPT completions divided by the number of TPT initiations in the previous semiannual period × 100; TPT coverage, calculated as the number of TPT completions divided by the total number of PLHIV eligible for TPT; and TB notification among PLHIV on ART, calculated as the number of registered new and relapsed TB patients with documented HIV-positive status divided by the total number of PLHIV on ART. TPT eligibility was defined as 95% of total PLHIV on ART; TPT ineligibility (5%) accounts for PLHIV with active TB and PLHIV discontinuing TPT because of loss to follow-up, death, or adverse events. Since October 2019, PLHIV have been considered to be on ART until <27 days after their last missed clinical appointment; clients whose last missed appointment was >28 days earlier are not considered to be receiving ART. Before October 2019, PLHIV were considered to be on ART until <90 days after their last missed appointment.
We used R software version 4.1.1 (The R Project for Statistical Computing, https://www.r-project.org) to analyze age groups, sex, and region. We described semiannual trends by using time series plots. We used nonparametric Cuzick tests to analyze TB notification rates across periods.
The total number of PLHIV on ART in Uganda increased from 890,938 in March 2017 to 1,283,662 in September 2022. Most (1,226,266; 95.5%) PLHIV were >15 years of age, and 822,864 (65.5%) were women. Age and sex distribution remained stable over time.
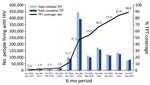
TPT completions increased from 28.6% (5,264/18,394) during October 2016–March 2017 to 94.0% (75,173/79,949) during October 2021–March 2022 (Table 1; Figure 1). We observed a steady increase in TPT completion rates except for a decline from 71.1% during April–September 2017 to 63.6% during October 2017–March 2018. The average regional TPT completion rate increased from 27.2% (interquartile range [IQR] 12.9%–41.9%) during October 2016–March 2017 to 93.8% (IQR 91.85%–96.25%) during October 2021–March 2022. The lowest regional average completion rate across all periods was 69.9% in the Kigezi region, and the highest average completion rate was 85.2% in the Lango region.
From October 2016–March 2017 through October 2021–March 2022, TPT coverage increased from 0.6% to 88.8% (Figure 2). In all periods, TPT coverage was higher for men. After October 2017–March 2018, TPT coverage increased steadily for both age groups; the largest increases were among PLHIV who were <15 years of age. The median regional TPT coverage during October 2021–March 2022 was 88.0% (IQR 84.5%–92.9%); the lowest rate (68.8%) was in the Karamoja region, and the highest rate (100.0%) was in the West Nile region.
TB notification rates increased from 881.1 cases/100,000 PLHIV during October 2016–March 2017 to 972.5 cases/100,000 PLHIV during October 2021–March 2022 (Table 2). Across all periods, TB notification rates were higher among men and PLHIV who were <15 years of age. During October 2021–March 2022, the highest regional TB notification rate was 1,819.2/100,000 PLHIV in the Karamoja region, and the lowest rate was 665.5/100,000 PLHIV in the Acholi region. The average regional TB notification rate during October 2016–March 2017 was 935.0 (IQR 715.4–1,069.9)/100,000 PLHIV compared with 1,032.72 (IQR 876.7–1,095.2)/100,000 PLHIV during October 2021–March 2022. Across all regions except Karamoja, TB notification rates declined during October 2019–March 2020.
In 6 years, Uganda successfully scaled up TPT coverage among a large cohort of PLHIV on ART. Key enablers of success were strong country leadership and ownership, integration of HIV and TB programs, data-driven stakeholder engagement, stable supply chains, and data use for continuous program improvement. However, TB notification rates increased, likely reflecting improvements in TB case reporting as part of efforts to provide TPT to all eligible PLHIV. Over time, TPT completion rates increased, especially during October 2019–March 2020, after the 100-day scale-up campaign (Appendix) (14). Although TPT coverage has continued to expand since 2020, negative effects of the COVID-19 pandemic are reflected by declines in TPT initiations and completions during the October 2019–March 2020 and April–September 2020 periods (3).
Considering available evidence (6–8), reducing the burden of TB among PLHIV in Uganda is feasible given high TPT coverage and if the following priorities are continued. First, full TPT coverage should be maintained, including among newly identified eligible PLHIV; shorter TPT regimens should be leveraged for high initiation and completion rates (15), and data should be routinely collected for close program monitoring. Second, enhanced TB case reporting is warranted, including among the general population, because the effects of high TPT coverage have not yet translated into declining TB notification rates among PLHIV. Ensuring early identification and treatment initiation for confirmed patients could include quality TB screening, testing, and prompt treatment. Third, newly recommended shorter TB treatment regimens should be considered standards of care to improve patient outcomes.
The first limitation of our study is that discrepancies were observed during some periods between disaggregated and overall totals because the national reporting systems integrated PEPFAR reporting requirements for TB-related data. Second, aggregate patient data are prone to ecologic fallacy and limited our ability to analyze person-level factors affecting TPT initiation and completion. Third, disaggregated data for TB cases during October 2016–March 2017 and October 2017–March 2018 were missing because of changes in data reporting requirements.
In summary, programmatic data indicate that almost all PLHIV in Uganda have received TPT, accelerating progress toward global targets for treatment coverage. Investments in timely TB screening, diagnosis, and earlier treatment during disease course should remain high priorities for TB/HIV prevention programming.
Dr. Lukoye is an epidemiologist in the Division of Global HIV and TB, Center for Global Health, US Centers for Disease Control and Prevention, Uganda. He serves as the public health expert for TB prevention, TB/HIV co-infections, and MDR TB and supports the Uganda Ministry of Health and implementing partners to achieve TB elimination.
Acknowledgments
We thank Fatumah Nalubega for technical advice and assisting in data analysis.
This project was reviewed in accordance with human research protection procedures at the CDC and was determined to be nonresearch. A waiver for informed consent was obtained from the Makerere University Institutional Review Board in Uganda to use programmatic data.
This publication was supported by cooperative agreement no. NU2GGH002093 (G.G.) from the CDC and the Public Health Institute. This study was supported by PEPFAR through CDC through a cooperative agreement (no. GH002221). PEPFAR attribution statement: This publication has been supported by PEPFAR through CDC. The findings and conclusions in this presentation are those of the author(s) and do not necessarily represent the official position of the funding agencies.
References
- Gupta RK, Lucas SB, Fielding KL, Lawn SD. Prevalence of tuberculosis in post-mortem studies of HIV-infected adults and children in resource-limited settings: a systematic review and meta-analysis. AIDS. 2015;29:1987–2002. DOIPubMedGoogle Scholar
- Granich R, Akolo C, Gunneberg C, Getahun H, Williams P, Williams B. Prevention of tuberculosis in people living with HIV. Clin Infect Dis. 2010;50(Suppl 3):S215–22. DOIPubMedGoogle Scholar
- World Health Organization. Global tuberculosis report 2022 [cited 2022 Aug 5]. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022
- UNAIDS. Joint United Nations Programme on HIV/AIDS. UNAIDS data 2021 [cited 2022 Aug 5]. https://www.unaids.org/sites/default/files/media_asset/JC3032_AIDS_Data_book_2021_En.pdf
- Ayele HT, Mourik MS, Debray TPA, Bonten MJM. Isoniazid prophylactic therapy for the prevention of tuberculosis in HIV infected adults: a systematic review and meta-analysis of randomized trials. PLoS One. 2015;10:
e0142290 . DOIPubMedGoogle Scholar - Briggs MA, Emerson C, Modi S, Taylor NK, Date A. Use of isoniazid preventive therapy for tuberculosis prophylaxis among people living with HIV/AIDS: a review of the literature. J Acquir Immune Defic Syndr. 2015;68(Suppl 3):S297–305. DOIPubMedGoogle Scholar
- Oxlade O, Rochon H, Campbell JR, Menzies D. Tuberculosis preventive treatment in people living with HIV-Is the glass half empty or half full? PLoS Med. 2021;18:
e1003702 . DOIPubMedGoogle Scholar - Pathmanathan I, Ahmedov S, Pevzner E, Anyalechi G, Modi S, Kirking H, et al. TB preventive therapy for people living with HIV: key considerations for scale-up in resource-limited settings. Int J Tuberc Lung Dis. 2018;22:596–605. DOIPubMedGoogle Scholar
- World Health Organization. Tuberculosis profile: Uganda. Estimates of TB burden, 2021 [cited 2022 Aug 5]. https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&entity_type=%22country%22&lan=%22EN%22&iso2=%22UG%22
- UNAIDS. Joint United Nations Programme on HIV/AIDS. Country factsheets Uganda 2021 [cited 2022 Aug 5]. https://www.unaids.org/en/regionscountries/countries/uganda
- Ministry of Health Republic of Uganda. Manual for management and control of tuberculosis and leprosy in Uganda, 3rd edition [cited 2022 Aug 5]. https://www.health.go.ug/cause/manual-for-management-and-control-of-tuberculosis-and-leprosy-in-uganda-3rd-edition
- Dirlikov E, Kamoga J, Talisuna SA, Namusobya J, Kasozi DE, Akao J, et al.; PEPFAR Uganda. Scale-up of HIV antiretroviral therapy and estimation of averted infections and HIV-related deaths—Uganda, 2004–2022. MMWR Morb Mortal Wkly Rep. 2023;72:90–4. DOIPubMedGoogle Scholar
- The Republic of Uganda Ministry of Health. Guidelines for programmatic management of TB preventive treatment in Uganda: a health worker guide. Kampala (Uganda): Government of Uganda, Ministry of Health; 2020.
- Ministry of Health Republic of Uganda. 100-Day accelerated isoniazid preventive therapy scale up plan, 2019 [cited 2022 Aug 5]. https://www.health.go.ug/cause/100-day-accelerated-isoniazid-preventive-therapy-scale-up-plan
- Semitala FC, Musinguzi A, Ssemata J, Welishe F, Nabunje J, Kadota JL, et al. Acceptance and completion of rifapentine-based TB preventive therapy (3HP) among people living with HIV (PLHIV) in Kampala, Uganda-patient and health worker perspectives. Implement Sci Commun. 2021;2:71. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: February 15, 2023
Table of Contents – Volume 29, Number 3—March 2023
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Deus Lukoye, US Centers for Disease Control and Prevention Uganda, US Embassy, 1577 Ggaba Rd, Nsambya, PO Box 7007, Kampala, Uganda
Top