Volume 4, Number 4—December 1998
Dispatch
Sporadic STEC O157 Infection: Secondary Household Transmission in Wales
Abstract
We conducted a study to quantify and characterize household transmission of Shiga toxin (Vero cytotoxin)– producing Escherichia coli O157 (STEC O157) following sporadic infection in Wales. Through total population surveillance, we identified 83 index case-patients and their household contacts. We screened fecal samples submitted from household contacts for STEC O157 and calculated the household transmission rate for sporadic STEC O157 infection to be 4% to 15%. Household contacts in groups at high risk (particularly children under 5 years of age) present a risk of spreading the infection in the wider community.
Shiga toxin–producing Escherichia coli O157 (STEC O157) infection causes severe enteric symptoms (hemorrhagic colitis with diarrhea, severe abdominal pain, and blood in the stools) (1) and hemolytic uremic syndrome (2% to 7% of cases) (2). The bacteria, which are from a predominantly bovine reservoir, are found in food or water (particularly beef products and milk) and are transmitted through zoonotic or environmental spread or person to person by the fecal-oral route (3). Fecal-oral transmission would explain why children with hemolytic uremic syndrome are seven times more likely than otherwise healthy children to have had close contact with a person with diarrhea in the 2 weeks before onset of illness (4).
Outbreaks attributed to person-to-person transmission have been confined mainly to children's day-care facilities and institutions providing care for the elderly or for those with physical or mental disabilities (5-8)—facilities in which hygiene is difficult to maintain—although an outbreak among siblings in a large family and a playmate has been described (9).
Most (90%) of STEC O157 cases reported in England and Wales are sporadic (10). Evidence suggests that the infectious dose is very low, perhaps as few as 10 organisms (11,12); hence the potential for person-to-person transmission among sporadic STEC O157 cases might be expected to be far greater than among sporadic cases of other common gastrointestinal pathogens. Although secondary spread of STEC O157 by sporadic cases has been reported (13), such transmission has not been accurately quantified or characterized on a population basis. This study aimed to quantify and characterize the secondary household transmission of STEC O157 from sporadic cases.
Cases (in persons residing in Wales and the English Borders) in which STEC O157 was isolated from initial fecal specimens and was subsequently confirmed by the Public Health Laboratory Service Laboratory of Enteric Pathogens were included in the study. Only the index case (i.e., the first to be recognized in a household) and sporadic cases (i.e., not part of a general outbreak) were included. Index case-patients were interviewed, face to face, by using a standard structured questionnaire to record age group, gender, onset, and hospitalization details. The names, as well as the age, gender, and occupation, of all household contacts were recorded in a confidential database.
Any person staying in the same household as a person with STEC O157 infection for one or more nights during the 7 days before disease onset and up to the interview date was considered a household contact. Diarrheal illness (defined as three or more loose stools in any 24-hour period during the 7 days before the onset of disease in the index patient and up to the date of the interview with the index patient) in the contact and the date of onset of the symptoms were also recorded. All household contacts were requested to provide one fecal specimen, which was examined as described (Table).
To determine whether the household contact cases were secondary or coprimary, the dates of disease onset for index case-patients were compared with those of their symptomatic household contacts. Also, the rates of infection in the households of index case-patients who had been hospitalized were compared with rates in households of patients who remained at home. We constructed matrices to determine the frequency of STEC O157 isolation for each age group of household contacts and index case-patients. The frequency of isolation of the organism from household contacts in the households of male index case-patients was compared with that from households of female index case-patients by calculating relative risks (RR) and Mantel-Haenszel chi squares. To determine any bias in the household contacts screened, we quantified factors affecting an individual contact's likelihood of submitting a fecal specimen (i.e., age, gender, and symptomatic status), as well as age and gender of index case-patient. We examined the delay between disease onset in the index case-patient and date of submission of specimens by contacts and compared the delays for household contacts of different ages. Household contacts infected with STEC O157 who belonged to certain groups (food handlers, health-care workers, children under 5 years of age, older children or adults unable to implement good hygiene) were considered a risk to the community, in accordance with current guidelines (14,15). The number of contacts falling into these groups was recorded.
Eighty-three persons considered index case-patients had 181 household contacts. Of the 181 contacts, 101 (56%) submitted fecal samples. Samples were submitted a median of 12 days after disease onset in the index case-patient (mean = 13.46 days; mode = 12 days; range = 6-40 days); timeliness of sample submission did not differ by age group. Of the 101 contacts examined, 15 had STEC-positive samples, giving a crude secondary household transmission rate of 15%. If it is assumed that contacts who did not submit fecal samples were not excreting STEC O157, the rate is 8% (15 of 181).
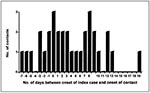
Of the 181 household contacts, 32 reported diarrhea: of these, 3 became ill on the same day as the index case-patient (none had confirmed STEC O157), 8 became ill before the index case-patient (2 had confirmed STEC O157), and 21 became ill after the index case-patient (7 had confirmed STEC O157) (Figure). If only the cases of household contacts who became ill after the index case-patient are considered secondary cases, the household transmission rate is 4% (7 of 181 cases).
STEC O157 were isolated from 15 of 109 contacts of case-patients under 14 years of age compared with 0 of 72 contacts of case-patients 15 years of age and older (p < 0.01) (Table). STEC O157 was no more likely to be isolated from male than female household contacts (8 of 95 versus 7 of 86, RR = 1.03, confidence interval [CI] = 0.39-2.73, p = 0.95). The contacts of male index case-patients were no more likely to have STEC-positive samples than those of female index case-patients (11 of 100 versus 4 of 81, RR = 2.23, CI = 0.74-6.73, p = 0.14). Among 53 parents of children with STEC O157, 2 (8%) of 24 fathers and 5 (17%) of 29 mothers had STEC-positive samples. Household contacts were more likely to be STEC positive if the index case-patient had not been hospitalized (12 of 102 versus 3 of 79, RR = 3.10, CI = 0.90-10.61, p = 0.05).
Seven household contacts were food handlers; five submitted samples, and none was STEC positive. Of 12 staff members at health-care facilities, 11 submitted samples, and none was STEC positive. Of 13 contacts who were children under 5 years of age attending a day-care facility, 11 submitted samples, and 2 were STEC positive. No household contacts were categorized as adults unable to implement good hygiene. Female household contacts were as likely as male to submit fecal samples (RR = 1.13, CI = 0.87-1.46, p = 0.37). Household contacts of female index case-patients were equally as likely as contacts of male patients to submit fecal specimens (RR = 0.81, CI = 0.62-1.06, p = 0.12).
Symptomatic contacts were more likely to submit specimens than asymptomatic contacts (81% [26/32] versus 50% [75/149], RR = 1.61 [1.28-2.03], p = 0.001) and also more likely to excrete STEC O157 than asymptomatic contacts (35% [9/32] versus 4% [6/149], RR = 6.98, CI = 2.67-18.24, p < 0.001 Fisher exact 2-tailed test).
The study showed that 8% to 15% of household contacts of persons with sporadic cases of STEC O157 were STEC positive. However, the household contacts could have had cases coprimary to the index case or even to the primary cases in the household. By excluding contacts who had symptoms before the index case-patient did and those who had no symptoms, we arrived at a household transmission rate of 4%.
The method of identifying secondary cases had certain biases. First, household contacts who had diarrheal symptoms were more likely to submit a stool sample, and their cases were therefore more likely to be recognized. As 40% of the secondary cases were asymptomatic, the true level of asymptomatic and mild infection in household contacts and overall secondary transmission were probably underestimated. This statement, however, does not take into account any role preexisting immunity might play in determining the severity of symptoms and the likelihood of fecal carriage. Persons with higher titers of immunoglobulin (Ig) G antibodies to VT1 in two family outbreaks of STEC have been more likely to be both asymptomatic and not excreting STEC than other family contacts with lower titers (16). Certain household contacts thus might not be able to contract secondary cases. Secondly, the age of the household contact is clearly associated with the likelihood of submitting a fecal sample. Younger contacts were more likely to be screened; therefore, their cases were more likely to be recognized. Nevertheless, the pattern of household transmission demonstrated using as the denominator 101 screened contacts was similar to that using all 181 contacts. The timeliness of specimens did not vary with age.
Overall, household contacts of 1 to 4 years of age and adults of 15 to 34 years of age are most likely to contract STEC O157 from an index case-patient. Children of 1 to 4 years of age explore the domestic environment and frequently put their hands (and other objects) in their mouths, and adults 15 to 34 years of age are likely to be looking after children with diarrhea. When we compared contacts who are parents of an infected child with the remainder of contacts, we observed an elevated risk of contracting STEC O157 in the home (not significant at the 10% level). The pattern of transmission suggests person-to-person spread by the fecal-oral route rather than by food.
Our findings have several implications for the control of STEC O157. Current U.K. guidelines (14,15) advise the prompt investigation of sporadic cases of STEC and the identification of other persons with symptoms in the household. Since STEC O157 is readily transmitted in the home, contacts of the index case-patient may excrete the organism and present a risk to the wider community through attendance at child day-care centers or through their occupations. Among household contacts, 2 of 13 children under 5 years of age who attended day care had STEC-positive samples. Our data support information from published outbreaks in day-care centers showing that children attending with diarrhea pose a major risk (8) and reinforcing U.K. guidelines (14,15) that, irrespective of symptoms, young siblings of an index case-patient under 5 years of age be excluded from day care until they have two negative fecal specimens at intervals not smaller than 48 hours.
Secondary spread of STEC O157 both during outbreaks and by sporadic cases has been documented (13,17,18). In a large hamburger-associated outbreak in the United States in 1993, an estimated 11% of all cases resulted from secondary spread (19). Whatever the source of the initial infection, secondary transmission, particularly by children, contributes significantly to the incidence of STEC O157 infection. Advice on the risk and on necessary hygienic precautions in the home when a family member has a diarrheal illness should be provided promptly to all affected persons.
Dr. Parry worked as an environmental health officer (sanitarian) for Cardiff City Council in infectious diseases and food safety. Since 1993 she has been a research officer with the Welsh Combined Centres for Public Health.
Dr. Salmon is a medical epidemiologist with the U.K. Public Health Laboratory Service Communicable Disease Surveillance Centre in Cardiff. He has a particular interest in zoonoses and has worked on the epidemiology of STEC infections for 10 years; in 1990 he created in Wales a system of total population surveillance for STEC O157.
Acknowledgments
We gratefully acknowledge the help and support of the following laboratories and their link personnel: Bronglais, Aberystwyth; Caerphilly Miners; East Glamorgan, Pontypridd; Llandough, Cardiff; Nevill Hall, Abergavenny; Prince Charles, Merthyr; Prince Phillip, Llanelli; Princess of Wales, Bridgend; Royal Gwent, Newport; Withybush, Haverfordwest; Wrexham Maelor; Bangor Public Health Laboratory (PHL); Cardiff PHL; Carmarthen PHL; Chester PHL; Hereford PHL; Rhyl PHL; Shrewsbury PHL; Swansea PHL; Laboratory of Enteric Pathogens, Central Public Health Laboratory, Colindale, London. We also thank the Welsh Office Standing Specialist Advisory Group (Microbiology): Local Authority Environmental Health Departments, health authority consultants in communicable disease control, and general practitioners throughout Wales and the Borders.
This work was funded by Department of Health (Grant 145).
References
- Riley LW, Remis RS, Helgerson SD, McGee HB, Wells J, Davis BR, Hemorrhagic colitis associated with a rare Escherichia coli serotype. N Engl J Med. 1983;308:681–5.PubMedGoogle Scholar
- Griffin PM. Escherichia coli O157:H7 and other enterohemorrhagic Escherichia coli. In: Blaser MJ, Smith PD, Ravdin JI, Greenberg HB, Guerrant RL, editors. Infections of the Gastrointestinal Tract. New York: Raven Press; 1995. p. 1-11.
- Griffin PM, Tauxe RV. The epidemiology of infections caused by Escherichia coli O157:H7, other entero-hemorrhagic E. coli, and the associated hemolytic uremic syndrome. Epidemiol Rev. 1991;13:60–98.PubMedGoogle Scholar
- Rower PC, Orrbine E, Lior H, Wells GA, McLaine PN. Canadian Pediatric Kidney Disease Reference Centre (CPKDRC) co-investigators. Diarrhea in close contacts as a risk factor for childhood haemolytic uraemic syndrome. Epidemiol Infect. 1993;110:9–16. DOIPubMedGoogle Scholar
- Kohli HS, Chaudhuri AKR, Todd WTA, Mitchell AAB, Liddell KG. A severe outbreak of E.coli O157 in two psychogeriatric wards. J Public Health Med. 1994;16:11–5.PubMedGoogle Scholar
- Carter AO, Borczyk AA, Carlson JAK, Harvey B, Hockin JC, Karmali MA, A severe outbreak of Escherichia coli O157:H7-associated hemorrhagic colitis in a nursing home. N Engl J Med. 1987;317:1496–500.PubMedGoogle Scholar
- Allaby MAK, Mayon-White R. Escherichia coli O157: outbreak in a day nursery. Commun Dis Rep CDR Rev. 1995;5:R4–6.PubMedGoogle Scholar
- Belongia EA, Osterholm MT, Soler JT, Ammend DA, Braun JE, MacDonald KL. Transmission of Escherichia coli O157:H7 infection in Minnesota child day-care facilities. JAMA. 1993;26:883–8. DOIGoogle Scholar
- Ludwig K, Ruder H, Bitzan M, Zimmermann S, Karch H. Outbreak of Escherichia coli O157 infection in a large family. Eur J Clin Microbiol Infect Dis. 1997;16:238–41. DOIPubMedGoogle Scholar
- Thomas A, Cheasty T, Frost JA, Chart H, Smith HR, Rowe B. Vero cytotoxin-producing Escherichia coli, particularly serogroup O157, associated with human infections in England and Wales. Epidemiol Infect. 1996;117:1–10. DOIPubMedGoogle Scholar
- Tilden J Jr, Young W, McNamara AM, Custer C, Boesel B, Lambert-Fair MA. A new route of transmission for Escherichia coli: infection from dry fermented salami. Am J Public Health. 1996;86:1142–5. DOIPubMedGoogle Scholar
- Willshaw GA, Thirlwell J, Jones AP, Parry S, Salmon RL, Hickey M. Vero cytotoxin-producing Escherichia coli O157 in beefburger linked to an outbreak of diarrhoea, haemorrhagic colitis and haemolytic uraemic syndrome in Britain. Lett Appl Microbiol. 1994;19:304–7. DOIPubMedGoogle Scholar
- E. coli O157 infections. SCIEH Weekly Report. 1995;29:57.
- Subcommittee of the Public Health Laboratory Service Working Group on Vero cytotoxin producing Escherichia coli (VTEC). Interim guidelines for the control of infections with Vero cytotoxin producing Escherichia coli (VTEC). Commun Dis Rep CDR Rev 1995;5(Review 6):R77-81.
- Working Party of the Public Health Laboratory Service Salmonella Committee. The prevention of human transmission of gastrointestinal infections, infestations, and bacterial intoxications. Commun Dis Rep CDR Rev 1995;5(Review 11):R158-72.
- Karmali M, Petric M, Winkler M, Bielaszewska M, Brunton J, van de Kar N, Enzyme-linked immunosorbent assay for detection of immunoglobulin G antibodies to Escherichia coli Vero cytotoxin 1. J Clin Microbiol. 1994;32:1457–63.PubMedGoogle Scholar
- Davis BS, Brogan RT. A widespread community outbreak of E. coli O157 infection in Scotland. Public Health. 1995;109:381–8. DOIPubMedGoogle Scholar
- Upton P, Coia JE. Outbreak of Escherichia coli O157 infection associated with pasteurised milk supply [Letter]. Lancet. 1994;344:1015. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Update: multistate outbreak of Escherichia coli O157:H7 infections from hamburgers—Western United States, 1992–1993. JAMA. 1993;269:2194–6. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 4, Number 4—December 1998
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
R.L. Salmon, PHLS-CDSC (Wales), Abton House, Wedal Road, Cardiff CF4 3QX, United Kingdom; fax: 44-0-1222-521987
Top