Volume 6, Number 2—April 2000
Dispatch
Haff Disease: From the Baltic Sea to the U.S. Shore
Abstract
Haff disease, identified in Europe in 1924, is unexplained rhabdomyolysis in a person who ate fish in the 24 hours before onset of illness. We describe a series of six U.S. patients from 1997 and report new epidemiologic and etiologic aspects. Although Haff disease is traditionally an epidemic foodborne illness, these six cases occurred in two clusters and as one sporadic case.
In the summer and fall of 1924, physicians near the Königsberger Haff shores along the Baltic coast recognized an outbreak of an illness characterized by sudden, severe muscular rigidity (1-3). No neurologic abnormalities, fever, splenomegaly, or hepatomegaly were observed (1). Patients often had coffee-colored urine. The clinical spectrum of disease varied, few patients died, and most survivors recovered quickly. In the following 9 years, similar outbreaks, affecting an estimated 1,000 persons, occurred seasonally in the summer and fall along the coast of the "haff" (a shallow lagoon). Recent ingestion of fish, usually cooked, was common among those who became ill; species of fish included burbot, eel, and pike. Seabirds and cats reportedly died after eating fish in the wild. Because of the absence of fever and the fact that fish had been cooked, known infectious causes were eliminated. Several toxic etiologies were proposed but could not be confirmed. Among these was arsenic poisoning (4), which is still cited in modern medical dictionaries as the cause of Haff disease (5). From 1934 until 1984, other outbreaks resembling Haff disease were described in Sweden and the Soviet Union (6-9). The first two cases reported in the United States occurred in Texas in June 1984; through 1996, only four more cases were reported: two from Los Angeles, California, in 1985, and two from San Francisco, California, in April 1986 (M. Tormey, pers. comm.). All patients had eaten buffalo fish before onset of illness. Tests of the remains of one of the fish meals suggested a neutral lipid as a causative agent. Reports of six cases of Haff disease from California and Missouri during a 5-month period (March-August) in 1997 prompted an investigation with the objectives of describing the epidemiology and clinical characteristics of the 1997 U.S. cases of Haff disease, tracing back implicated fish, and elucidating the cause of Haff disease.
Based on the clinical description of the original cases from 1924 to 1933, we defined a case of Haff disease as illness in a person with unexplained rhabdomyolysis who had eaten fish in the 24 hours before onset of symptoms. The laboratory marker used to define rhabdomyolysis was a fivefold or greater elevation in creatine kinase (CK) levels, with a muscle/brain (MB) fraction <5% (10). Cases were identified through county and state epidemiologists, as well as the Food and Drug Administration (FDA) laboratories in Bothell, Washington, and Dauphin Island, Alabama. We interviewed all persons with cases reported to the Los Angeles County Health Department or FDA. We reviewed medical records for demographic information, medical history, course of illness, and food exposures, including method of preparation and source of food purchase. For the California cases (March 8-9 and August 8), we conducted active surveillance in city or community hospitals near the case-patients' residence during the 5 days surrounding the dates of onset. Surveillance included reviews of laboratory logs (for cases with highly elevated CK but a low MB fraction) and emergency room logs for all patients with a diagnosis of suspected fish poisoning.
State and local environmental management staff visited stores and markets where fish was bought to trace the implicated fish lots. We interviewed fish wholesalers regarding the number and location of fishermen catching buffalo fish. Because fish eaten by the patients originated from Louisiana and Missouri, we discussed with health departments and environmental experts possible sources of fish intoxication. Recovered leftovers and uncooked fish from the same lot were tested for sodium channel-active biotoxins (e.g., ciguatoxin [the toxin of ciguatera] or saxitoxin [the toxin of paralytic shellfish poisoning]), and cyanobacterial toxins (e.g., microcystin or nodularin, which are toxins of blue-green algae) (11,12). Samples from the Bakersfield case were tested for organophosphates, and other samples were tested for arsenic.
To characterize the physicochemical properties of the toxin, extract from both cooked and uncooked fish was partitioned into water-soluble, nonpolar lipid (hexane) and polar lipid (chloroform) fractions. These fractions were then administered intraperitoneally and orally to laboratory mice. Fractions causing toxicity to mice were further analyzed for identification of the toxin.
From March through August 1997, two clusters of Haff disease cases occurred in Los Angeles, California, and St. Louis, Missouri (13); one isolated case occurred in Bakersfield, California. The Los Angeles cluster consisted of two sisters who lived together and a third patient who was admitted to the same hospital during the same weekend. The St. Louis cluster was a married couple. The four meals, all eaten at home, contained buffalo fish. Six (75%) of the eight persons who ate buffalo fish became ill. All patients were >30 years of age (33 to 87 years); five were Ukrainian immigrants, and one was African-American. Three of the six patients were taking medications, including aspirin, codeine, and simvastatin, that could have exacerbated rhabdomyolysis. Two persons who vomited shortly after the meal had either milder symptoms or lower laboratory values. The median incubation time to onset of symptoms after fish ingestion was 8 hours (6 to 21 hours). All patients were hospitalized, none died, and the median hospital stay was 3 days. Clinically, five of six patients had rapid onset of generalized muscular pain and rigidity, so severe that in one case ventilation was required (Table). In one patient who had chest pain only, the diagnosis of Haff disease was made through the exclusion of other causes of chest pain and the epidemiologic link with two other case-patients who had eaten buffalo fish purchased from the same market.
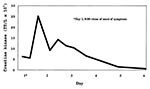
The predominant laboratory abnormalities were elevated CK and myoglobin. Other muscle enzymes, such as glutamate oxalate transaminase, glutamate pyruvate transaminase, and lactate dehydrogenase, were also elevated. The CK was elevated to a mean of 12,700 IU/L (normal is usually <300 IU/L) (Figure). At the peak of the CK, the MB fraction was <5% in all cases. The mean maximum myoglobin level, tested in three patients, was 6,997 IU/L (upper limit of normal 100 IU/L). Treatment consisted of intravenous fluids, in addition to mannitol or bicarbonate. Several of the patients had variable sequelae, including weakness and fatigue, for several months after the acute stage. Active surveillance has identified no further cases.
Buffalo fish (Ictiobus cyprinellus) is a bottom-feeding freshwater fish similar to carp. The fish was fried (four cases) or cooked for 3.5 hours as "gefilte fish" (two cases). Fish were purchased locally either in a supermarket (California) or alive from a fish tank at a market (Missouri). Fish lots were caught by approximately 25 commercial fishermen from rivers in Louisiana (three incidents) or five fishermen in rivers and lakes near St. Louis, Missouri (one incident). No specific bodies of water could be identified as the origin of implicated fish. No fish or unusual animal die-off was noted in the areas where buffalo fish were caught.
Tests of the fish for toxins were either negative or below toxicity thresholds. The fact that the eaten fish was thoroughly cooked suggests that the presumed toxin is heat-stable. Mice fed hexane-soluble products extracted from cooked fish had behavioral changes consistent with muscle impairment; bladders contained red-brown urine.
Historically, Haff disease has been identified during seasonal outbreaks in Europe. This report documents that it may also occur sporadically or in small clusters. Ten of the 12 U.S. cases of Haff disease reported since 1984 occurred during March through August (M. Tormey, pers. comm.). All patients had eaten buffalo fish before becoming ill; 8 of the 12 patients were California residents, although the buffalo fish was caught in Louisiana or Missouri waters.
Most reported cases or outbreaks of Haff disease have been associated with freshwater fish, unlike most other seafood-related illnesses (e.g., ciguatera, scombroid fish poisoning, or paralytic shellfish poisoning), which are associated with saltwater fish (14). The clinical symptoms of Haff disease also differ from those of any other fish-related toxic or bacterial illness. Symptoms of rhabdomyolysis predominate and neurologic features are absent, in contrast to ciguatera or the various forms of shellfish poisoning (14). Because of the spectrum of symptoms, the potential for misdiagnosis is considerable. Furthermore, an increasing number of health-conscious persons prefer diets that include fish. In 1998, more than 4 billion pounds of fish, both domestic and imported, were eaten in the United States (website of National Oceanic and Atmospheric Administration: www.nmfs.org). Unusual smell or taste does not help identify toxic fish, and normal cooking methods cannot detoxify a fish capable of causing Haff disease. Because Haff disease may occur not only in epidemics but also in small clusters or sporadically, fish consumption should be included in the history of patients with unexplained rhabdomyolysis.
Dr. Buchholz, who was an officer in the Epidemic Intelligence Service, Centers for Disease Control and Prevention, at the time of this study, is a medical epidemiologist with the Los Angeles County Department of Health Services. His interests include foodborne disease epidemiology, outbreak investigations, and surveillance for listeriosis and influenza.
Acknowledgment
We thank Steve Musser, Martin Robl, James Ahlrep, and Richard Honkanen for laboratory support; Doug Dodson, Diane Rackers, Louise McFarland, Al Medina, Michael Tormey, and S.B. Werner for their advice and help; Piotr Kramarz for his translation of Russian articles; and the staff of the Kern County Health Department, particularly Drs. Dulan, Talbot, and Steve Terrell-Perica, for their cooperation and tireless support in the investigation.
References
- Zu Jeddeloh B. Haffkrankheit [Haff disease]. [Ger]. Ergebnisse in der inneren Medizin 1939;57:138-82.
- Assmann H, Bielenstein H, Habs H, zu Jeddeloh B. Beobachtungen und Untersuchungen bei der Haffkrankheit 1932 [Observations and investigations about Haff disease 1932]. [Ger]. Dtsch Med Wochenschr. 1933;I:122–6. DOIGoogle Scholar
- Lentz O. Über die Haffkrankheit [About Haff disease]. [Ger]. Med Klin. 1925;I:4–8.
- Lockemann G. Chemische Untersuchungen zur Haffkrankheit [Chemical investigations about Haff disease]. [Ger]. Biochem Z. 1929;207:194–216.
- Taylor EJ, ed. Dorland's illustrated medical dictionary. 28th ed. Philadelphia: W.B. Saunders Co.; 1994. Disease, Haff: 483.
- Leschenko PD, Khoroshilova NV, Slipchenko LM, Kaznachei RY. Observation of Haff-Üchs disease cases. [Rus]. Vopr Pitan. 1965;24:73–6.PubMedGoogle Scholar
- Strusevich AV. Haff-Iuksov-Sartlan Disease. [Alimentary-toxic paroxysmal myoglobinuria]. [Rus]. Arkh Patol. 1966;28:56–60.PubMedGoogle Scholar
- Sidorova LD. Iuksovsk-Sartlansk disease. Kidney lesions in dietary and toxic paroxysmal myoglobinuria. [Rus]. Ter Arkh. 1985;57:120–3.PubMedGoogle Scholar
- Salluzzo RF. Rhabdomyolysis. In: Rosen P, Barkin R, editors. Emergency medicine: concepts and clinical practice. 4th ed. St. Louis: Mosby-Year Book; 1997. p. 2478-87.
- Manger RL, Leja LS, Lee SY, Hungerford JM, Hokama Y, Dickey RW, Detection of sodium channel toxins: directed cytotoxicity assays of purified ciguatoxins, brevetoxins, saxitoxins, and seafood extracts. J AOAC Int. 1995;78:521–7.PubMedGoogle Scholar
- Honkanen RE, Mowdy DE, Dickey RW. Determination of DSP-toxins, okadaic acid and dinophysis toxin-1 in shellfish by Serine/Threonin Protein Phosphatase Assay. J AOAC Int. 1996;79:1336–43.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. Haff disease associated with eating buffalo fish—United States, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:1091–3.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. Tetrodotoxin poisoning associated with eating puffer fish transported from Japan—California, 1996. MMWR Morb Mortal Wkly Rep. 1996;45:389–91.PubMedGoogle Scholar
Figure
Table
Cite This ArticleTable of Contents – Volume 6, Number 2—April 2000
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Udo Buchholz, Los Angeles County Department of Health Services, Acute Communicable Disease Control, 313 N. Figueroa St., Room 212, Los Angeles, CA 90012, USA; fax: 213-482-4856
Top