Volume 7, Number 2—April 2001
THEME ISSUE
4th Decennial International Conference on Nosocomial and Healthcare-Associated Infections
Introduction
Infection Control and Changing Health-Care Delivery Systems
Abstract
In the past, health care was delivered mainly in acute-care facilities. Today, health care is delivered in hospital, outpatient, transitional care, long-term care, rehabilitative care, home, and private office settings. Measures to reduce health-care costs include decreasing the number of hospitals and the length of patient stays, increasing outpatient and home care, and increasing long-term care for the elderly. The home-care industry and managed care have become major providers of health care. The role of specialists in health-care epidemiology has changed accordingly.
Over the past two decades, there has been a revolution in health-care delivery systems in the United States. The number of acute-care facilities has decreased, the proportion of patients requiring intensive care in acute-care facilities has increased, and the number of surgical procedures performed in outpatient settings or surgical centers has increased. Not only has there been a shift to the outpatient setting, but the long-term care, home-care, and managed-care industries have grown dramatically. I will provide an overview of recent changes in the U.S. health-care delivery system and describe the challenges for health-care epidemiology and infection control departments in the new millennium.
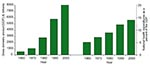
In the 1970s and 1980s, the acute-care facility was the center of the hospital infection and infection control universe (1) (Figure 1). Most health care was delivered in the acute-care setting, and outpatient, long-term, and home care were relatively small, in number of facilities and patients. The growth of the U.S. gross domestic product (GDP) and the proportion spent on health care reflect change in health-care delivery (Figure 2). From 1960 to 2000, the GDP grew nearly 15-fold, from approximately $526 billion to nearly $8,000 billion. At the same time, the proportion of the GDP expended on health care increased from 5.1% (approximately $27 billion) to 14% (approximately $1,120 billion)--a 41% increase. This growth, together with the introduction of the prospective payment plan based on diagnostic-related groups, led to marked changes in hospitalization (Table). From 1975 to 1995, the number of hospitals decreased from 7,126 to 6,291, the number of hospital beds decreased from 1.47 million to 1.08 million, patient admissions decreased by 5%, hospital stay decreased by 36%, the average length of patient stay decreased by 33%, and the number of inpatient surgical procedures decreased by 27%. These trends have resulted in fewer and smaller hospitals, more and larger intensive-care units, and greater severity of illness in the hospitalized population. At the same time, reports of nursing shortages and downsizing of infection control departments have been increasing, despite the fact that nearly 2 million hospital-acquired infections occur each year. Thus, the challenge for infection control departments in acute-care settings will be to focus surveillance activities on populations at high risk, calculate risk-adjusted rates of hospital-acquired infection, and provide feedback to appropriate personnel so that integrated prevention programs can be implemented and interventions evaluated to ensure quality health care (2–4).
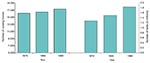
Since 1950, the number of persons >65 years of age in the United States has nearly tripled, from 12.2 million to 36 million. To accommodate this growth, the number of nursing homes increased from 16,091 in 1986 to 17,208 in 1996, and the number of beds in these facilities increased from 1.298 million to 1.839 million (Figure 3) (5). By 2035, the population of persons 65 years of age will exceed 80 million. In 1997, 1,600,000 persons lived in long-term care facilities; by 2005, this figure will increase to an estimated 5,000,000. Since 3%-15% of such patients acquire an infection in these facilities each year, the 48,000 to 240,000 infections estimated to have occurred in 1997 will increase to an estimated 150,000 to 750,000 in 2005.
Challenges for infection control in long-term care facilities include the following: First, many facilities have no dedicated infection control personnel to conduct surveillance and lead prevention, education, and intervention programs. Second, uniform definitions and surveillance protocols are needed for infections acquired in long term-care facilities. Third, further studies are needed to determine the best numerator (e.g., number of infections, colonization, positive cultures, symptomatic or asymptomatic residents) and denominator (e.g., number of residents, number of resident-days, number of residents with a specific device or device-days) to use for infection rate calculations to facilitate inter- and intrafacility comparisons. Fourth, for many reasons, including lack of availability of laboratory facilities, failure of clinicians to order appropriate diagnostic work-ups, and inadequate reimbursement for diagnostic testing for infections, patients in long-term-care facilities often are not evaluated for infection when they are symptomatic. (Rather, antimicrobial drugs are initiated on an empiric basis.) The influence of this reduced testing on detection of infections acquired in long-term-care facilities needs to be assessed.
The fastest-growing segment of the health-care delivery system has been the home health business. In 1988, the Health Care Financing Administration expended approximately $2 billion for home health. By 1999, approximately $20 billion was expended. Today, almost as many persons receive health care in the home (an estimated 34,000,000 annually) as in acute-care settings.
Infection control in home-care settings poses the following challenges: 1) Few home health-care companies have dedicated infection control personnel. 2) No uniform definitions of infection or protocols for infection surveillance have been agreed upon. 3) Often health-care delivery in the home is uncontrolled and may even be provided by family members. 4) Health Care Financing Administration reimbursement schedules largely determine policies on the frequency of home health-care visits. 5) For some infection rates, such as central venous catheter-associated bloodstream infections, device-adjusted rates are needed for intra- and interfacility and company comparisons. Who will collect these data? How will the numerator (number of infections) be captured when the data may come from various sources, including the hospital, private physician offices, or private laboratories? Often these data are not reported to the home health-care company and thus may be very difficult to obtain. Although collecting these data from a single home health-care company is easier, many acute-care facilities contract with 10 to 20 home health-care companies and do not require in their contracts that such data (numerator, denominator, or rates) be provided. Thus, further studies are necessary to determine the data critical for measuring the quality of home health-care delivery and to identify which components of our infection control programs are essential.
At least initially, home health care and other infection control personnel should focus their efforts on high-risk infections, e.g., urinary tract, bloodstream, pneumonia, or skin and soft tissue infections. For specific infections, e.g., urinary tract and bloodstream infections, device-specific infection rates should be calculated. Uniform definitions applicable to home care, uniform surveillance protocols, and a national nonpunitive reporting system should be established so that rates can be compared.
Since 1976, managed care and health maintenance organizations in the United States have grown explosively. In 1976, there were approximately 174 health maintenance organizations in the United States (Figure 4) (5). By 2000, that number had grown to >700. Concomitantly, the number of persons enrolled in such plans increased from 6 million to >75 million, and the percentage of the U.S. population enrolled in such plans increased tenfold, from 2.8% to 29%. Because managed-care organizations focus their efforts on cost containment, the challenge for infection control personnel will be to demonstrate to administrative personnel that both quality care and cost containment are facilitated by improving infection surveillance and control programs.
From 1993 to 1996, the annual number of visits to hospital outpatient clinics increased from 62.5 million to 67.1 million, the number of hospital emergency department visits remained stable at approximately 90 million, and the number of physician office visits increased from 717 million to 734 million. Challenges for infection control personnel in outpatient and ambulatory-care settings include determining for which infections to conduct surveillance, what definitions to use, who will conduct the surveillance, to whom the data will be reported, and who will be responsible for implementing the changes. Often infection control personnel are not aware of what populations of patients are being seen or what procedures are being performed in outpatient settings. Furthermore, no systems are in place to collect the needed numerators (infections or adverse events) and denominators (e.g., number of patients with central venous catheters being seen in the clinic) data. To collect the data for these rate calculations, it will be necessary to identify methods, including electronic databases, whereby such data can be captured and used. Calculating infection or adverse event rates in outpatients and reporting them to ambulatory care and specialty personnel (e.g., the director of the oncology clinic) will be useful for improving education programs for health-care workers, as well as the quality of patient care.
Infection control personnel play a critical role in preventing infections and medical errors. They conduct infection surveillance in acute-care facilities, apply standard definitions and surveillance protocols, calculate infection rates, report these data to essential personnel, implement prevention interventions, and evaluate their impact. Most importantly, as the Study of the Efficacy of Infection Control Programs (SENIC) has documented, the infection surveillance and prevention efforts of these infection control personnel are cost effective (6).
Increasingly, infection control personnel have been expanding their activities to include prevention of infection and other adverse events in long-term care, home-care, and outpatient settings. If we are to prevent infections and other adverse events associated with the delivery of health care in the entire spectrum of health-care settings, we will need to expand the infection control departments in all these settings (Figure 5).
Over the past two decades, acute-care facilities have become smaller and fewer, but the hospitalized patient population has become more severely ill and more immunocompromised and thus at greater risk for hospital-acquired infections. At the same time, the proportion of the U.S. population >65 years of age has increased, as have the number of long-term care facilities and the number of beds in these facilities. This trend is expected to continue for the next 50 years. Similarly, delivery of health care in the home has become the most rapidly growing sector of the health-care system. Currently, nearly as many patients are receiving care in the home as in the inpatient setting. Provision of health care in managed-care and outpatient and ambulatory-care settings continues to expand. Thus, the spectrum of health-care delivery in 2000 is larger than ever before. Because of the severely ill and immunocompromised populations in these settings, prevention of infections and other adverse events is a major component of providing quality care.
In each of these settings, challenges need to be addressed. In acute-care settings, where the responsibilities of infection control departments already have markedly expanded (e.g., occupational health, prevention exposure to bloodborne pathogens, prevention of Mycobacterium tuberculosis or multidrug-resistant bacterial transmission, medical errors) during the past 2 decades, emphasis will need to be on conducting surveillance of populations at high risk, calculating device-specific infection rates, and educating health-care workers on infection control. In long-term-care facilities, infection control personnel need to establish infection surveillance systems, determine baseline infection rates for comparison, improve device and antimicrobial drug use, and educate staff about prevention. In managed-care settings, infection control personnel will need to expand their efforts toward cost-effective infection surveillance and control programs. In the outpatient and ambulatory setting, infection control personnel will need to work with computer systems and clinic personnel to design information systems to improve collection of data about infections and other adverse events so that rates can be calculated and trends monitored. Because of their expertise in epidemiologic methods, infection control personnel can assist infection control, quality assurance, and medical error reduction programs in all these health-care system components.
Infection control personnel will need to expand their efforts to match the expansion of the health-care delivery system. Enhanced administrative support for programs to prevent infections and medical errors will be needed if we are to reduce the risk of infection and other adverse events and improve the quality of care in the entire spectrum of health-care delivery. Now, instead of the acute-care facility being the center of the infection control universe, the infection control department has become the center of the diverse health-care delivery system. Infection control departments will need to expand their surveillance of infections and adverse events and their prevention efforts to all settings in which health care is delivered.
Dr. Jarvis is associate director for program development, Division of Healthcare Quality Promotion (currently Hospital Infections Program), CDC, and president of the Society for Healthcare Epidemiology of America (SHEA).
References
- Martone WJ, Garner JS. Proceedings of the Third Decennial International Conference on Nosocomial Infections. Am J Med. 1991;91(3B):1S–333S. DOIPubMedGoogle Scholar
- Jarvis WR, Edwards JR, Culver DH, Hughes JM, Horan TC, Emori TG, Nosocomial infection rates in adult and pediatric intensive care units in the United States. Am J Med. 1991;91(3B):185S–91S. DOIPubMedGoogle Scholar
- Gaynes RP, Martone WJ, Culver DH, Emori TG, Horan TC, Banerjee SN, Comparison of rates of nosocomial infections in neonatal intensive care units in the United States. Am J Med. 1991;91(3B):192S–6S. DOIPubMedGoogle Scholar
- Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Surgical wound infection rates by wound class, operative procedure, and patient risk index. Am J Med. 1991;91(3B):152S–7S. DOIPubMedGoogle Scholar
- Kramarow E, Lentzner H, Rooks R, Weeks J, Sayday S. Health and aging chartbook: health, United States, 1999. Hyattsville (MD): National Center for Health Statistics, U.S. Department of Health and Human Services.
- Haley RW, Culver DH, White JW, Morgan WM, Emori TG. The efficacy of infection surveillance and control programs in preventing nosocomial infections in U.S. hospitals. Am J Epidemiol. 1985;121:182–205.PubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 7, Number 2—April 2001
| EID Search Options |
|---|
|
|
|
|
|
|



Please use the form below to submit correspondence to the authors or contact them at the following address:
William R. Jarvis, Hospital Infections Program, MS E-69, Centers for Disease Control and Prevention, 1600 Clifton Road, Atlanta, GA 30333; fax: 404-639-6459
Top