Volume 9, Number 1—January 2003
Research
Natural Enzootic Vectors of Venezuelan equine encephalitis virus in the Magdalena Valley, Colombia
Abstract
To characterize the transmission cycle of enzootic Venezuelan equine encephalitis virus (VEEV) strains believed to represent an epizootic progenitor, we identified natural vectors in a sylvatic focus in the middle Magdalena Valley of Colombia. Hamster-baited traps were placed into an active forest focus, and mosquitoes collected from each trap in which a hamster became infected were sorted by species and assayed for virus. In 18 cases, a single, initial, high-titered mosquito pool representing the vector species was identified. These vectors included Culex (Melanoconion) vomerifer (11 transmission events), Cx. (Mel.) pedroi (5 transmissions) and Cx. (Mel.) adamesi (2 transmissions). These results extend the number of proven enzootic VEEV vectors to 7, all of which are members of the Spissipes section of the subgenus Melanoconion. Our findings contrast with previous studies, which have indicated that a single species usually serves as the principal enzootic VEEV vector at a given location.
Venezuelan equine encephalitis (VEE) is an emerging zoonotic arboviral disease that affects equines and humans in the Americas (1). Venezuelan equine encephalitis virus (VEEV) has caused sporadic outbreaks since the early part of the 20th century, with some epidemics affecting >100,000 persons. For many years, the source of the epizootic/epidemic VEEV strains belonging to subtypes IAB and IC viruses remained unknown. After antigenically related but distinct, equine-avirulent, enzootic strains of VEEV were isolated in the 1960s, researchers hypothesized that epizootic/epidemic strains evolve from enzootic VEEV progenitors (2). The first genetic evidence supporting this hypothesis came from RNA fingerprinting studies that indicated a close relationship between subtype ID–enzootic VEEV strains from Colombia and epizootic/epidemic isolates belonging to subtype IC (3). Later, sequencing (4) and phylogenetic (5,6) studies also supported the evolution of the epizootic/epidemic serotype IAB and IC strains from enzootic ID VEEV progenitors. Recently, comprehensive phylogenetic analyses have indicated that the epizootic/epidemic strains evolved independently on at least three occasions from a single lineage of ID VEEV that circulates in eastern and central Colombia, western Venezuela, and northern Peru (7–10). Other ID-like VEEV lineages that occur in Panama, Amazonian Peru, southwestern Colombia, coastal Ecuador, north-central Venezuela, and Florida have not generated any of the epizootic/epidemic strains sequenced (10–12).
Enzootic VEEV (subtypes ID–IF, II–VI) circulate nearly continuously in sylvatic or swamp habitats in various tropical and subtropical locations in the New World (1,13). These viruses generally use small mammals as their reservoir hosts and are transmitted by mosquitoes. Enzootic mosquito vectors have been identified for four VEEV variants: 1) Culex (Melanoconion) portesi transmits Mucambo virus (VEE complex subtype IIIA) in Trinidad (14), 2) Cx. (Mel.) cedecei transmits Everglades virus (VEE complex subtype II) in southern Florida (15), 3) Cx. (Mel.) aikenii sensu lato (ocossa and panocossa) transmits subtype ID VEEV in Panama (16,17), and 4) Cx. (Mel.) taeniopus (formerly opisthopus) is the primary enzootic vector of subtype IE VEEV in Guatemala (18). More than 70% of enzootic field isolations have come from the subgenus Melanoconion, suggesting that these mosquitoes are the principal vectors of most or all enzootic VEE complex strains (17).
The infrequency of VEE emergence is probably determined by the infrequent, simultaneous occurrence in time and space of viral mutations that mediate host range changes, combined with ecologic and epidemiologic conditions that permit efficient amplification (1). To understand the mechanisms of VEE emergence from enzootic progenitors in Colombia and Venezuela, we are studying the hosts in which epizootic mutations may occur and in which the selection of epizootic strains may follow. However, the vector and reservoir hosts of the particular subtype ID VEEV lineage implicated in epizootic emergence have not been identified. Using an efficient system of vector identification employing hamster baited traps, we identified Cx. (Mel.) vomerifer, Cx. (Mel.) pedroi, and Cx. (Mel.) adamesi as natural enzootic vectors in an active focus of subtype ID VEEV in the middle Magdalena Valley of Colombia.
Study Area
The study was carried out from 1999 to 2000 in the Monte San Miguel Forest in the middle Magdalena Valley of Colombia (6° 23′ 30′′N; 74° 21′ 41′′ W; 50 m elevation). This is a lowland tropical rainforest surrounded by cattle ranches created by deforestation. Mean minimum and maximum daily temperatures are 23°C and 33°C (overall mean of 29°C), respectively, and annual rainfall averages 2,700 mm. Mean relative humidity is 80%. Generally, the peaks of the rainy seasons occur in April–May and October–November. Numerous previous isolations of subtype ID VEEV from sentinel hamsters (9) indicate that this forest site is a stable enzootic focus.
Mosquito Traps
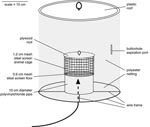
Hamster-baited traps were used for detection of natural VEEV vectors. These traps were a version of the Trinidad No. 10 trap (19) with the following modifications: 1) the metal can comprising the trap opening was replaced by a polyvinyl chloride pipe, 9 cm in diameter; 2) the cylindrical animal cage was enlarged to 11 cm in diameter and 12 cm in height; 3) the roof was constructed from plexiglass; and 4) the opening for mosquito aspiration was a simple buttonhole sewn into the polyester collection net (Figure). The traps were baited with adult golden Syrian hamsters obtained from a colony maintained at the Instituto Nacional de Salud in Bogota. Baited traps were suspended approximately. 1.5 m above the ground and placed in transects at 10-m intervals. Carrots and rat chow were provided for food and water. The traps were checked each morning between 0600 and 0800 h, and some were also checked in the evening between 1700 and 1900 h. Mosquitoes were removed from the traps by using an aspirator, and the daily or semi-daily collections from each trap were frozen as a single pool in a plastic bottle immersed in liquid nitrogen vapor. When hamsters within the traps became moribund or died, serum samples were obtained by cardiac puncture or their hearts were dissected aseptically and frozen for virus isolation.
Detection of Natural Transmission to Hamsters
To confirm VEEV infection in dead or moribund hamsters, virus was isolated from a 10% heart tissue suspension in Eagle’s minimal essential medium (MEM), supplemented with 20% fetal bovine serum (FBS) and antibiotics. The suspension was prepared in a Ten Broeck tissue grinder and centrifuged at 15,000 x g for 5 min; 200 μL of the supernatant was added to a 25-cm2 flask containing a monolayer of Vero cells and adsorbed for 1 h at 37°C; 6 mL of additional MEM containing 2% FBS was then added. Cultures were incubated at 37°C for 5 days or until cytopathic effects were evident.
Mosquito pools from traps in which hamster infection with VEEV was confirmed were assayed for infectious virus. Pools containing 1–40 individuals of each mosquito species were triturated with a Minibeadbeater (BioSpec Products, Inc., Bartlesville, OK) or a Ten Broeck tissue grinder containing 1.0 mL of MEM supplemented with 20% FBS, penicillin, streptomycin, and amphotericin B. The triturated pool was centrifuged for 5 min at 15,000 x g, and 200 µl of the supernatant was added to a 10-mL plastic tube or a 25-cm2 cell culture dish containing a monolayer of Vero cells and 2–5 mL of MEM. Cultures were monitored for cytopathic effects for 5 days.
Genetic and Antigenic Characterization of VEEV Isolates
Viruses isolated from hamster heart tissue suspensions and mosquito pools were characterized antigenically by using immunofluorescence of infected cells and a panel of monoclonal antibodies described previously (20). Subtype ID VEEV isolates were further characterized genetically by reverse transcription–polymerase chain reaction (PCR) amplification of an 856-nucleotide portion of the PE2 (sometimes called p62) envelope glycoprotein precursor gene as described previously (8), followed by single-stranded conformation polymorphism (SSCP) or sequence analysis (9). For SSCP analysis, PCR products were purified on agarose gel by using the QIAquick Gel Extraction Kit (QIAGEN, Valencia, CA). A 2-μl volume of the PCR amplicon DNA suspension was mixed with 8 μl of SSCP loading buffer (95% formamide, 0.05% bromophenol blue, and 0.05% xylene cyanol). The DNA was heated to 95°C for 5 minutes, rapidly cooled on ice, loaded onto an 8% polyacrylamide gel, and underwent electrophoresis in 1X Tris-borate EDTA buffer at room temperature for 20 h at 8 mA. Single-stranded DNA products were visualized by using silver staining (21). SSCP patterns were compared by measuring the migration of single-stranded DNA of the various isolates in comparison to one another and to a standard DNA ladder.
For vector identification studies, 87 hamsters were exposed in traps within the Monte San Miguel Forest for 5–7 days. Of these, 38 became moribund or died and were processed for virus isolation. VEEV was isolated from 37 hamsters, and the mosquito collections from the corresponding traps were assayed for virus.
In 18 of the traps yielding infected hamsters, a vector species was identified by using the following criteria: 1) the hamster died at least 24 h after the collection of the presumed vector, consistent with the incubation time of VEEV in hamsters (22); 2) during the first day in which infected mosquitoes were collected from the trap, only one species pool had a high titer (>5.0 log10 PFU/pool) consistent with an infectious mosquito, as determined by previous experimental studies of enzootic VEEV vectors (18,23–26); 3) the remaining pools, from the first day in which infected mosquitoes were collected, were uninfected, or had low titers (<5.0 log) shown previously to be inconsistent with an infectious mosquito (18,23–26); 4) the mosquito collections on the days subsequent to that of the vector collection were mostly infected, reflecting hamster viremia and the ingestion of infectious blood by mosquitoes biting >12 h after the transmission event; and 5) virus isolates from the hamster and corresponding vector were indistinguishable antigenically and genetically with SSCP analysis, sequencing, or both. In 18/37 infected hamster events studied, these criteria were fulfilled, vector was identified unambiguously. Typical data for one of these transmission events (hamster 164) is shown in Table 1. In this example, transmission by Cx. vomerifer occurred < 24 h after exposure of the trap, and the vector pool had a titer of 5.8 log10 PFU/pool. The other two infected pools from day 2, Cx. pedroi and Aedes serratus, had log titers <3.3, indicating that they were not capable of transmission. These pools presumably contained one or more mosquitoes that engorged on the hamster after viremia began, probably just before the daily trap collection. On the next day, all mosquito pools contained infectious virus in their midguts, representing viremic hamster blood ingested by mosquitoes within the trap.
A total of 18 transmission events were characterized as described above. The most common interval of collection of the identified vector was 24–48 h after exposure, reflecting a very high level of enzootic VEEV transmission in the Monte San Miguel Forest. Cx. vomerifer was implicated in 11 of these events, Cx. pedroi in 5, and Cx. adamesi in 2 transmissions (Table 2). The minimum infection/transmission rate for the mosquitoes we collected could not be determined directly because we did not identify the mosquito collections for traps where transmission to the hamster did not occur. However, rates on the order of 1/200–1/1000 can be estimated for these three vector species if the species composition is assumed to be similar in traps where transmission did not occur. Even if this assumption is incorrect, the error in this estimate should not be more than twofold because VEEV transmission occurred in most traps.
Use of Hamster-Baited Traps for Arbovirus Vector Identification
Traditional criteria for arthropod vector identification include the following: 1) demonstration of feeding or other effective contact with pathogen’s host; 2) association in time and space of the vector and pathogen; 3) repeated demonstration of natural infection of the vector, and 4) experimental transmission of the pathogen by the vector (27). Infection rates for arbovirus vectors tend to be relatively low, usually <1%. Therefore, fulfillment of these criteria for arbovirus vectors usually relies on the capture of large numbers of arthropods for virus isolation, followed by experimental laboratory transmission studies to ensure that species found infected in nature are competent vectors. Although this strategy is the most comprehensive and unbiased, it is extremely costly and time consuming, accounting for the relative paucity of information on natural vectors of many arboviruses. Some studies of VEEV vectors have also relied on oral infection from experimentally infected hamsters with viremia levels of very high titer, on the order of 8 log10 PFU/mL (28,29), a titer at least 100–1,000 times greater than that generated by experimentally infected rodent reservoir hosts (30,31), equines (13,30,32), or naturally infected humans (8,33) (Some studies of equine viremia have yielded titers of >108 suckling mouse intracerebral 50% lethal doses, but this method for quantifying VEEV titers is 100- to 1000-fold more sensitive than PFU [30,34]). Results from these studies are therefore inconclusive regarding natural transmission potential.
Other investigators have streamlined the vector identification process by collecting suspected vectors and sorting them according to species, then exposing single-species pools to naïve animals in a field or laboratory setting to detect transmission (16,18). We have taken this approach one step further by combining collection and transmission detection using hamster-baited traps. This method simplifies the vector identification process in several ways: 1) Hamster-baited traps attract and capture only arthropod species that are attracted to small mammals, the natural reservoir hosts of the enzootic VEEV (Proechimys spp. spiny rats in the case of subtype ID VEEV circulating in this focus [35]), minimizing collection and mosquito processing efforts. 2) Arthropod collections from traps where no transmission occurs do not need to be sorted, greatly reducing a laborious step in the vector identification process. 3) Only a small number of arthropod pools must be tested for virus, eliminating much of the cost, labor, and biosafety hazard associated with traditional vector identification approaches. In addition, the hamster-baited traps can serve as sentinels for detection of active virus circulation in a forest and reveal the presence of other viruses in a focus. However, unlike other sentinel enclosures that allow arthropods to escape after biting a viremic bait animal and thereby initiate artificial amplification, the hamster-baited traps capture most of the arthropods that bite the viremic host and prevent most or all artificial amplification. A similar strategy for detecting transmission of western equine encephalitis and St. Louis encephalitis viruses to chickens in baited traps was described by Reeves et al. (36).
Using these hamster-baited traps alone, we were not able to measure directly the capture efficiency of our traps. However, in the case of five infected hamsters, the lack of any collections with a single or few high titer mosquito species pools on the day preceding total infection of collected mosquitoes indicates that the arthropod responsible for transmission may have escaped. In other cases, two or more mosquito pools collected on the first day virus was detected had titers consistent with infectious vectors, precluding vector identification. We are currently experimenting with funnel-shaped openings to reduce the frequency of vector escape from this trap design. As with any passive trap design, a compromise between ease of vector entry and frequency of escape must be sought to maximize collections.
Enzootic Vectors of Venezuelan Equine Encephalitis Complex Viruses
Previous studies of VEE complex enzootic transmission have each identified a single, principal mosquito species in a given geographic region. All of these species, including Cx. portesi (14), Cx. cedecei (15), Cx. aikenii sensu lato (ocossa and panocossa) (16,17), and Cx. taeniopus (18) are members of the Spissipes section of the subgenus Melanoconion within the genus Culex (37). Previous studies of enzootic VEEV transmission in the Catatumbo region of northeastern Colombia also suggested that Cx. pedroi might be the principal vector, based on abundance in active foci (38). Cx. vomerifer from Iquitos, Peru, also has been shown to be susceptible to infection by several strains of VEEV (28), but was only tested after mosquitoes ingested 8 log10 PFU/mL from viremic hamsters, a viremia titer at least 100 times greater than that generated by experimentally infected rodent reservoir hosts (30,31). Our findings of at least three enzootic vectors of subtype ID VEEV in Colombia contrast with the findings of all previous studies of enzootic VEEV vectors, which suggested that enzootic VEEV strains are each adapted to a single, principal vector species (13,18,39–41). In Colombia, subtype ID VEEV appears to utilize efficiently both Cx. vomerifer and Cx. pedroi in the Magdalena Valley. Cx. adamesi, which is usually less abundant in the Monte San Miguel Forest, appears to serve as a secondary vector.
All three of the mosquito species that we identified as VEEV vectors are members of the Spissipes section of the subgenus Culex (Melanoconion), bringing the total to seven confirmed vectors within this section of closely related mosquitoes. The genetic or ecologic basis for the exclusive use of these mosquitoes by enzootic VEE complex viruses deserves further study. Hypotheses to explain this phenomenon include possible shared, derived characteristics of the Spissipes section, such as particularly high susceptibility to infection by enzootic VEE complex viruses, a particularly high degree of association with the Proechimys spp (35). and other small mammalian reservoir hosts (13), or both. Mosquito longevity and population sizes in habitats that support large populations of reservoir hosts may also favor transmission by members of the Spissipes section (35).
Role of Enzootic Vectors in VEEV Emergence and Disappearance
Identification of the principal enzootic vectors (Cx. vomerifer and Cx. pedroi) of subtype ID VEEV strains believed to be closely related to epizootic progenitors will allow us to assess the role of these mosquitoes in the generation of mutations that mediate VEE emergence by enhancing equine viremia and infection of epizootic mosquito vectors such as Ae. taeniorhynchus. The hypothesis that epizootic VEEV is not recovered from sylvatic foci because these strains lose their fitness for the enzootic vectors (25) can also be tested in the two principal vectors that we identified.
Dr. Weaver is director for Tropical and Emerging Infectious Diseases, Center for Biodefense and Emerging Infectious Diseases, and professor in the departments of Pathology, Microbiology, and Immunology, at the University of Texas Medical Branch, Galveston. His research interests focus on the ecology, epidemiology, evolution, and pathogenesis of arthropod-borne viruses, especially Venezuelan equine encephalitis and dengue viruses, as well as mosquito-virus interactions.
Acknowledgments
We thank Marco Fidel Suarez and Eutimio Guerra for excellent technical assistance.
This research was supported by grants AI39800 and AI48807 from the National Institutes of Health, and by Colciencias grant 2104-04-758-98.
References
- Weaver SC. Recurrent emergence of Venezuelan equine encephalomyelitis. In: Scheld WM, Hughes J, editors. Emerging infections I. Washington (DC): ASM Press; 1998. p. 27–42.
- Johnson KM, Martin DH. Venezuelan equine encephalitis. Adv Vet Sci Comp Med. 1974;18:79–116.PubMedGoogle Scholar
- Rico-Hesse R, Roehrig JT, Trent DW, Dickerman RW. Genetic variation of Venezuelan equine encephalitis virus strains of the ID variety in Colombia. Am J Trop Med Hyg. 1988;38:195–204.PubMedGoogle Scholar
- Kinney RM, Tsuchiya KR, Sneider JM, Trent DW. Genetic evidence that epizootic Venezuelan equine encephalitis (VEE) viruses may have evolved from enzootic VEE subtype I-D virus. Virology. 1992;191:569–80. DOIPubMedGoogle Scholar
- Rico-Hesse R, Weaver SC, de Siger J, Medina G, Salas RA. Emergence of a new epidemic/epizootic Venezuelan equine encephalitis virus in South America. Proc Natl Acad Sci U S A. 1995;92:5278–81. DOIPubMedGoogle Scholar
- Weaver SC, Bellew LA, Rico-Hesse R. Phylogenetic analysis of alphaviruses in the Venezuelan equine encephalitis complex and identification of the source of epizootic viruses. Virology. 1992;191:282–90. DOIPubMedGoogle Scholar
- Wang E, Barrera R, Boshell J, Ferro C, Freier JE, Navarro JC, Genetic and phenotypic changes accompanying the emergence of epizootic subtype IC Venezuelan equine encephalitis viruses from an enzootic subtype ID progenitor. J Virol. 1999;73:4266–71.PubMedGoogle Scholar
- Weaver SC, Salas R, Rico-Hesse R, Ludwig GV, Oberste MS, Boshell J, Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. Lancet. 1996;348:436–40. DOIPubMedGoogle Scholar
- Moncayo AC, Medina GM, Kalvatchev Z, Brault AC, Barrera R, Boshell J, Genetic diversity and relationships among Venezuelan equine encephalitis virus field isolates from Colombia and Venezuela. Am J Trop Med Hyg. 2001;65:738–46.PubMedGoogle Scholar
- Powers AM, Oberste MS, Brault AC, Rico-Hesse R, Schmura SM, Smith JF, Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis from a single genotype of enzootic subtype ID virus. J Virol. 1997;71:6697–705.PubMedGoogle Scholar
- Salas RA, Garcia CZ, Liria J, Barrera R, Navarro JC, Medina G, Ecological studies of enzootic Venezuelan equine encephalitis in north-central Venezuela, 1997–1998. Am J Trop Med Hyg. 2001;64:84–92.PubMedGoogle Scholar
- Brault AC, Powers AM, Holmes EC, Woelk CH, Weaver SC. Positively charged amino acid substitutions in the E2 envelope glycoprotein are associated with the emergence of Venezuelan equine encephalitis virus. J Virol. 2002;76:1718–30. DOIPubMedGoogle Scholar
- Walton TE, Grayson MA. Venezuelan equine encephalomyelitis. In: Monath TP, editor. The arboviruses: epidemiology and ecology, vol. IV. Boca Raton (FL): CRC Press; 1988. p. 203–31.
- Aitken THG. Habits of some mosquito hosts of VEE (Mucambo) virus from northeastern South America, including Trinidad. In: Proceedings of workshop-symposium on Venezuelan encephalitis virus. Washington: Pan American Health Organization; Scientific Publ. 243;1972. p. 254–6.
- Chamberlain RW, Sudia WD, Coleman PH, Work TH. Venezuelan equine encephalitis virus from south. Fla Sci. 1964;145:272–4.
- Galindo P, Grayson MA. Culex (Melanoconion) aikenii: natural vector in Panama of endemic Venezuelan encephalitis. Science. 1971;172:594–5. DOIPubMedGoogle Scholar
- Galindo P. Endemic vectors of Venezuelan encephalitis. In: Proceedings of workshop-symposium on Venezuelan encephalitis virus, Washington: Pan American Health Organization; Scientific Publ. 243; 1972. p. 249–53.
- Cupp EW, Scherer WF, Ordonez JV. Transmission of Venezuelan encephalitis virus by naturally infected Culex (Melanoconion) opisthopus. Am J Trop Med Hyg. 1979;28:1060–3.PubMedGoogle Scholar
- Davies JB. A small mosquito trap for use with animal or carbon dioxide baits. Mosq News. 1971;31:441–3.
- Roehrig JT, Bolin RA. Monoclonal antibodies capable of distinguishing epizootic from enzootic varieties of subtype I Venezuelan equine encephalitis viruses in a rapid indirect immunofluorescence assay. J Clin Microbiol. 1997;35:1887–90.PubMedGoogle Scholar
- Black WC, Vanlandingham DL, Sweeney WP, Wasieloski LP, Calisher CH, Beaty BJ. Typing of LaCrosse, snowshoe hare, and Tahyna viruses by analyses of single-strand conformation polymorphisms of the small RNA segments. J Clin Microbiol. 1995;33:3179–82.PubMedGoogle Scholar
- Scherer WF, Dickerman RW, Chia CW, Ventura A, Moorhouse A, Geiger R, Venezuelan equine encephalitis virus in Veracruz, Mexico, and the use of hamsters as sentinels. Science. 1963;145:274–5. DOIGoogle Scholar
- Scherer WF, Cupp EW, Lok JB, Brenner RJ, Ordonez JV. Intestinal threshold of an enzootic strain of Venezuelan equine encephalomyelitis virus in Culex (Melanoconion) taeniopus mosquitoes and its implication to vector competency and vertebrate amplifying hosts. Am J Trop Med Hyg. 1981;30:862–9.PubMedGoogle Scholar
- Weaver SC, Scherer WF, Cupp EW, Castello DA. Barriers to dissemination of Venezuelan encephalitis viruses in the Middle American enzootic vector mosquito, Culex (Melanoconion) taeniopus. Am J Trop Med Hyg. 1984;33:953–60.PubMedGoogle Scholar
- Scherer WF, Weaver SC, Taylor CA, Cupp EW. Vector incompetency: its implication in the disappearance of epizootic Venezuelan equine encephalomyelitis virus from Middle America. J Med Entomol. 1986;23:23–9.PubMedGoogle Scholar
- Weaver SC, Scherer WF, Taylor CA, Castello DA, Cupp EW. Laboratory vector competence of Culex (Melanoconion) cedecei for sympatric and allopatric Venezuelan equine encephalomyelitis viruses. Am J Trop Med Hyg. 1986;35:619–23.PubMedGoogle Scholar
- Barnett HC. The incrimination of arthropods as vectors of disease. Proceedings of the 11th Congress on Entomology, Vienna, Austria. 1960;2:341–5.
- Turell MJ, Jones JW, Sardelis MR, Dohm DJ, Coleman RE, Watts DM, Vector competence of Peruvian mosquitoes (Diptera: Culicidae) for epizootic and enzootic strains of Venezuelan equine encephalomyelitis virus. J Med Entomol. 2000;37:835–9. DOIPubMedGoogle Scholar
- Turell MJ, Barth J, Coleman RE. Potential for Central American mosquitoes to transmit epizootic and enzootic strains of Venezuelan equine encephalitis virus. J Am Mosq Control Assoc. 1999;15:295–8.PubMedGoogle Scholar
- Wang E, Bowen RA, Medina G, Powers AM, Kang W, Chandler LM, Virulence and viremia characteristics of 1992 epizootic subtype IC Venezuelan equine encephalitis viruses and closely related enzootic subtype ID strains. Am J Trop Med Hyg. 2001;65:64–9.PubMedGoogle Scholar
- Young NA, Johnson KM, Gauld LW. Viruses of the Venezuelan equine encephalomyelitis complex experimental infection of Panamanian rodents. Am J Trop Med Hyg. 1969;18:290–6.PubMedGoogle Scholar
- Walton TE, Alvarez O, Buckwalter RM, Johnson KM. Experimental infection of horses with enzootic and epizootic strains of Venezuelan equine encephalomyelitis virus. J Infect Dis. 1973;128:271–82.PubMedGoogle Scholar
- Bowen GS, Calisher CH. Virological and serological studies of Venezuelan equine encephalomyelitis in humans. J Clin Microbiol. 1976;4:22–7.PubMedGoogle Scholar
- Martin DH, Dietz WH, Alvaerez O Jr, Johnson KM. Epidemiological significance of Venezuelan equine encephalomyelitis virus in vitro markers. Am J Trop Med Hyg. 1982;31:561–8.PubMedGoogle Scholar
- Barrera R, Ferro C, Navarro JC, Freier J, Liria J, Salas R, Contrasting sylvatic foci of Venezuelan equine encephalitis virus in northern South America. Am J Trop Med Hyg. 2002;67:324–34.PubMedGoogle Scholar
- Reeves WC, Bellamy RE, Scrivani RP. Differentiation of encephalitis virus infection rates from transmission rates in mosquito vector populations. Am J Hyg. 1961;73:303–15.PubMedGoogle Scholar
- Sirivanakarn S. A review of the systematics and proposed scheme of internal classification of the New World subgenus Melanoconion of Culex (Diptera: Culicidae). Mosquito Systematics. 1982;14:265–333.
- Dickerman RW, Cupp EW, Groot H, Alarcon AM, Cura E, Dickerman AW, Venezuelan equine encephalitis virus activity in northern Colombia during April and May 1983. Bull Pan Am Health Organ. 1986;20:276–83.PubMedGoogle Scholar
- Scherer WF, Weaver SC, Taylor CA, Cupp EW, Dickerman RW, Rubino HH. Vector competence of Culex (Melanoconion) taeniopus for allopatric and epizootic Venezuelan equine encephalomyelitis viruses. Am J Trop Med Hyg. 1987;36:194–7.PubMedGoogle Scholar
- Cupp EW, Kreutzer RD, Weaver SC. The biosystematics of Culex (Melanoconion) taeniopus sensu lato in relation to Venezuelan equine encephalomyelitis. Mosquito Systematics. 1989;21:216–21.
- Weaver SC. Vector biology in viral pathogenesis. In: Nathanson N, editor. Viral pathogenesis. New York: Lippincott-Raven; 1997. p. 329–52.
Figure
Tables
Cite This ArticleTable of Contents – Volume 9, Number 1—January 2003
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Scott Weaver, Keiller 4.128, Department of Pathology, University of Texas Medical Branch, Galveston, Texas 77555-0609, USA; fax: 409-747-2415
Top