Volume 23, Number 6—June 2017
Research Letter
Ebola Virus Imported from Guinea to Senegal, 2014
Abstract
In March 2014, the World Health Organization declared an outbreak of Ebola virus disease in Guinea. In August 2014, a case caused by virus imported from Guinea occurred in Senegal, most likely resulting from nonsecure funerals and travel. Preparedness and surveillance in Senegal probably prevented secondary cases.
Ebola virus disease (EVD) is a hemorrhagic fever caused by Ebola virus (EBOV); the mortality rate is high (1,2). EBOV was discovered in 1976, simultaneously in Zaire (now the Democratic Republic of the Congo) and Sudan (3,4). Since then, small to large outbreaks have occurred sporadically in the Democratic Republic of the Congo, Sudan, Gabon, Uganda, Côte d’Ivoire, and Congo (5–7).
In March 2014, the World Health Organization (WHO) reported an EVD outbreak caused by Zaire EBOV in Guinea (8,9). The main feature of this outbreak was its extension into urban areas and neighboring countries (Liberia, Sierra Leone, Nigeria, Senegal, Mali). Ten countries on 3 continents were affected; 28,646 confirmed, probable, and suspected cases and 11,323 deaths were recorded.
In August 2014, Senegal was the fifth country in Africa to be affected by imported EBOV (10). We described this case, the patient’s itinerary and epidemiologic links with confirmed case-patients in Guinea, and the evolution of the disease and the virus.
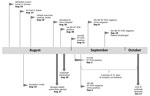
The patient was a 21-year-old man from Forecariah, Guinea, who had traveled by land to Senegal during the night of August 13–14, 2014. The date of his illness onset was August 16, 2014; symptoms were fever, vomiting, diarrhea, yellow or black feces, anorexia, and asthenia. On August 18, he visited a suburban medical center in the suburbs of Dakar, where he received treatment for malaria: quinine, antipyretic and antimicrobial medications, and intravenous rehydration. Diarrhea and vomiting stopped on day 4 after illness onset, but fever and asthenia persisted. On August 26, the patient was admitted to Fann Hospital, Dakar, with slight dehydration, fever (39.2°C), and herpetic lesions. Because no epidemiologic link with EVD was established, the patient was not isolated.
On August 27, a total of 12 members of the patient’s family, all suspected of having EVD, were admitted to an Ebola treatment center in Conakry, Guinea; test results indicated EBOV positivity for 6. Epidemiologic investigation indicated that a member of this family had traveled to Dakar and was hospitalized. The Epidemic Management Committee set up by WHO in Guinea established an epidemiologic link between the patient in Fann Hospital and the confirmed case-patients in Guinea and quickly informed the health authorities in Senegal. The patient in Fann Hospital finally acknowledged that he had attended his uncle’s nonsecure funeral in Guinea on August 10, before coming to Dakar (Figure).
On August 28, the man was transferred to an isolation center, and blood samples were sent to the Institut Pasteur laboratory in Dakar, a WHO-approved collaborating Centre for EBOV diagnostics. Real-time reverse transcription PCR (RT-PCR) was positive for Zaire EBOV; viral load was 2.04 × 104 genome copies/mL. ELISA of the same sample detected Zaire EBOV–specific IgM (titer 1:400) and IgG (titer 1:3,200). This case of EVD in Senegal was reported to WHO on August 29. The patient received supportive care, and his clinical course progressed well; on August 31, he was apyrexic and his asthenia had decreased. In terms of virus evolution, a second blood sample tested on day 18 after illness onset showed diminution of viral load (4.96 × 103 genome copies/mL) and an IgG titer increase to 1:6,400. A third blood sample collected on day 20 showed a negative RT-PCR result, but a urine sample collected the same day showed a positive result with a viral load of 2.04 × 104 genome copies/mL. RT-PCRs of blood and urine collected on days 24 and 34 were negative, and serologic analyses showed a high IgG titer (1:12,800).
The patient was declared cured on September 18, 2014. Epidemiologic investigations revealed a total of 74 contacts in Senegal, including 41 healthcare workers (from the suburban medical center and Fann Hospital). Symptoms developed in 5 of these contacts, but their test results were negative for EBOV. No secondary case was detected after 42 days of monitoring, and the outbreak in Senegal was declared over on October 17, 2014, with only 1 confirmed case reported.
The case-patient’s low viral load, detected during the first RT-PCR 10 days after illness onset, probably explains the absence of secondary cases in Fann Hospital. However, the absence of secondary cases in the suburban medical center that the patient had visited on days 3–4 after illness onset and among the family members in Dakar is a rare feature of EVD. The preparedness and surveillance established in Senegal after announcement of EVD in Guinea led to training of healthcare workers for proper use of protective equipment and security procedures with any patient, which probably prevented virus spread in the suburban medical center. This case of EBOV importation from Guinea to Senegal confirms the problems encountered with Ebola outbreak management, including the roles of nonsecure funerals and travel in virus spread.
Dr. Ka is an infectious disease physician who works in the Infectious and Tropical Diseases Clinic, Fann Hospital, Dakar, Senegal. His research interests are EVD, HIV, and hepatitis. Dr. Fall is a virologist who works at Arbovirus and Viral Hemorrhagic Fever Unit, Institut Pasteur de Dakar, Senegal. Her research interests include arbovirus–vector interactions, mechanisms of arbovirus transmission, and public health activities such as diagnosis of arboviruses and hemorrhagic fever viruses.
Acknowledgments
We thank Moussa Dia, El Hadji Abdourahmane Faye, Ousmane Kébé, Khardiata Mbaye, Davy Evrard Kiori, and Oumar Ndiaye for their excellent technical assistance in laboratory diagnosis.
This work was supported by grants from the Institut Pasteur de Dakar, Senegal, and the Ministry of Health, Senegal.
References
- Cenciarelli O, Pietropaoli S, Malizia A, Carestia M, D’Amico F, Sassolini A, et al. Ebola virus disease 2013-2014 outbreak in west Africa: an analysis of the epidemic spread and response. Int J Microbiol. 2015;2015:769121. DOIPubMedGoogle Scholar
- Feldmann H, Klenk HD. Filoviruses. In: S. Baron, editor. Medical Microbiology, 4th ed. Galveston (TX): University of Texas Medical Branch; 1996.
- World Health Organization. Report of an International Commission: Ebola haemorrhagic fever in Zaïre, 1976. Bull World Health Organ. 1978;56:271e93.
- World Health Organization/International Study Team. Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team. Bull World Health Organ. 1978;56:247–70.PubMedGoogle Scholar
- Centers for Disease Control and Prevention. Outbreaks chronology: Ebola virus disease [cited 2015 Aug 2]. http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html
- World Health Organization. Ebola virus disease [cited 2015 Nov 28]. http://www.who.int/mediacentre/factsheets/fs103/en/
- Colebunders R, Borchert M. Ebola haemorrhagic fever—a review. J Infect. 2000;40:16–20. DOIPubMedGoogle Scholar
- World Health Organization. Ebola virus disease in Guinea [cited 2015 Aug 18]. http://www.who.int/csr/don/2014_03_23_ebola/en
- Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, et al. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med. 2014;371:1418–25. DOIPubMedGoogle Scholar
- World Health Organization. Ebola virus disease update—Senegal [cited 2014 Nov 15] http://www.who.int/csr/don/2014_08_30_ebola/en/
Figure
Cite This Article1These authors contributed equally to this article.
2These authors contributed equally to this article.
Table of Contents – Volume 23, Number 6—June 2017
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Ousmane Faye, Virology Pole, Institut Pasteur de Dakar, BP 220 Dakar, Senegal
Top