Volume 29, Number 9—September 2023
Dispatch
High Prevalence of Candida auris Colonization during Protracted Neonatal Unit Outbreak, South Africa
Abstract
One third of patients were colonized by Candida auris during a point-prevalence survey in a neonatal unit during an outbreak in South Africa. The sensitivity of a direct PCR for rapid colonization detection was 44% compared with culture. The infection incidence rate decreased by 85% after the survey and implementation of isolation/cohorting.
Candida auris has been recognized as a critical priority pathogen globally, causing invasive infections and persistent outbreaks in healthcare facilities (1). In June 2019, an outbreak dominated by C. auris clade III occurred in a 185-bed neonatal unit of a national central hospital located in Gauteng Province, South Africa. To contain the outbreak, multiple infection prevention and control (IPC) measures were implemented (Appendix), including colonization screening for contact patients housed in the same cubicle as babies who had positive cultures. Despite those measures, sustained control was not achieved, similar to the case for other prolonged outbreaks (2,3). Although small section-wide colonization point-prevalence surveys (PPS) were conducted earlier for control (Figure 1), a comprehensive unit-wide PPS was never undertaken. We describe a unit-wide PPS conducted before the neonatal unit was relocated to a new facility as part of a longstanding renovation plan.
Institutional ethics approval for public health surveillance and outbreak investigations was granted by the University of the Witwatersrand HREC (Medical) (M210752). Permission to conduct the survey was granted by the hospital’s Medical Advisory Committee, Chief Executive Officer, and the Paediatric Department management.
The aim of the PPS was to reduce C. auris transmission in the new facility. The PPS was conducted on November 2, 2021 (3 days before the relocation), to establish colonization status and implement cohorting/isolation for affected infants. We used a direct reverse transcription PCR (RT-PCR)‒based method for rapid detection and compared this to culture as the reference standard. We collected composite skin swab specimens from the axilla and groin (4) and used selective and enrichment methods to isolate C. auris in culture (Appendix). We used the one-step SYBR PrimeScript RT-PCR Kit II (TaKaRa Bio, Inc., https://www.takarabio.com), according to Sexton et al. (5).
We swabbed 195 infants; RT-PCR results for 55 (93%) of 59 infants admitted to the neonatal intensive care unit and transitional care unit were available within 24 hours of specimen collection. Samples from those sections were prioritized because of high previous number of infections (Appendix Figure 1). Processing of the remaining swab samples was completed within 48 hours. The prevalence of C. auris colonization by RT-PCR was 15% (29/195) (Table 1). All culture results were available within 17 days after specimen collection because of multiple processing steps (Appendix Figure 2). With culture, the prevalence of C. auris was 32% (63/195). The overall prevalence was 33% (64/195). The sensitivity of the RT-PCR compared with culture was 44% (95% CI, 32%–58%). The sensitivity was highest in the high-care surgical unit and the neonatal intensive care unit, where the prevalence of colonization was highest on the day of the unit-wide PPS (Table 2).
All infants who were colonized with C. auris were immediately placed in isolation/cohorted in a separate section with contact precautions after either a positive PCR result or culture result. Infants who were positive for C. auris based on PPS results or who had a previous culture-positive diagnostic specimen for C. auris were not transferred to the new facility. Instead, they remained in the isolation/cohorting section of the old neonatal unit until discharge. Because swab specimen culture results were still unknown on the relocation day, admitted PCR-negative and subsequently admitted infants were housed in separate wings in the new unit. Apart from that measure and the allocation of dirty and clean equipment areas, IPC practices in the new unit remained largely unchanged.
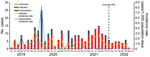
Using archived laboratory data, we analyzed incidence rates of C. auris infection (isolation from normally sterile specimens) or colonization (isolation from nonsterile specimens) in the unit before the PPS (January 1, 2019–November 2, 2021) and after the PPS and relocation (November 3, 2021–June 24, 2022) (Figure 2). Before the PPS, 167 new cases of C. auris infection were diagnosed, an incidence rate of 1.3 cases/1,000 patient-days. After the survey, 27 new cases of infection were diagnosed, an 85% decrease in the infection incidence rate to 0.2 cases/1,000 patient-days after PPS. The incidence rate of C. auris colonization was 0.6 cases/1,000 patient-days (n = 82) before the PPS and 0.1 cases/1,000 patient-days after (n = 4).
Compared with previous limited surveys in the unit, we determined a high prevalence of C. auris colonization during the unit-wide PPS, probably a major factor in ongoing transmission within the neonatal unit (6,7). Screening of direct contacts and surveys limited to specific sections of the unit probably missed colonized patients in other areas, and our results emphasize the need for routine unit-wide surveys, which are more effective in detecting the true extent of colonization during protracted C. auris outbreaks.
In the months after the unitwide PPS, infection and colonization incidence decreased. However, infections and colonization (albeit to a lesser extent) continued to occur. Assuming that skin colonization always precedes invasive infection, the continued occurrence of C. auris infections suggests the PPS was only partially successful at control. Culture-based methods used for identification delayed implementation of contact precautions because of a long turnaround time. The RT-PCR intended for rapid identification of colonization had a lower sensitivity than the >90% reported previously (5). The low observed sensitivity was possibly caused by low fungal load in the swab specimens, supported by a longer time-to-culture-positivity for PCR-negative/culture-positive swab specimens than for PCR-positive/culture-positive swab specimens (Appendix Table 1). In addition, a higher fungal burden on patient skin in high-prevalence neonatal unit sections might have improved detection (7). Nonetheless, we could not exclude PCR inhibitors as a reason for low sensitivity because our assay lacked an internal control.
Despite the limitations of our case detection methods during the PPS, the substantial decrease in infection incidence strongly suggests that the PPS and related IPC measures played a crucial role in control. Although colonization incidence also decreased after the PPS, we are uncertain whether that was a real decrease. The incidence in the period before the PPS included colonized patients identified during limited surveys, resulting in more colonization cases potentially being detected in that period compared with the post-PPS period.
Undetected colonization and persisting IPC challenges, such as staff shortages and bed occupancy in excess of capacity, all probably contributed to the continued transmission within the unit. Topical chlorhexidine gluconate or terbinafine could lead to skin decolonization (8,9). However, determining the optimal skin concentration, required contact time, and number of applications for sustained C. auris clearance and ensuring safety in neonatal populations remain unresolved (10). A comprehensive bundle of IPC measures, which includes routine PPS to assess skin colonization, preferably using a more sensitive PCR method (such as TaqMan chemistry) (7,11), along regular audits of adherence to contact precautions, surgical aseptic technique, device care protocols, and periodic environmental sampling to guide cleaning and decontamination efforts, should be implemented. This system could be challenging and costly to maintain in a large unit; however, these measures are crucial for control. In conclusion, regular PPS should be conducted in neonatal units experiencing ongoing C. auris outbreaks to identify colonized persons and implement IPC precautions to prevent spread.
Ms. Shuping is an epidemiologist at the Centre for Healthcare-Associated Infections, Antimicrobial Resistance and Mycoses at the National Institute for Communicable Diseases, Johannesburg, South Africa. Her primary research interests are neonatal infection epidemiology, antimicrobial resistance, and infection prevention and control.
Acknowledgments
We thank Inge Kleinhans, Husna Ismail, Amanda Shilubane, Silondiwe Nzimande, Dikeledi Kekana, and Siphiwe Kutta for providing support during the PPS; the neonatal unit nursing staff for helping to plan the survey; and the National Institute for Communicable Diseases Surveillance Information Management Unit for providing surveillance data throughout the outbreak investigation.
This work was supported by the National Institute for Communicable Diseases. a division of the National Health Laboratory Service.
References
- World Health Organization. WHO fungal priority pathogens list to guide research, development and public health action. Oct 25, 2022 [cited 2023 Jul 10]. https://www.who.int/publications/i/item/9789240060241
- Ruiz-Gaitán A, Moret AM, Tasias-Pitarch M, Aleixandre-López AI, Martínez-Morel H, Calabuig E, et al. An outbreak due to Candida auris with prolonged colonisation and candidaemia in a tertiary care European hospital. Mycoses. 2018;61:498–505. DOIPubMedGoogle Scholar
- Eyre DW, Sheppard AE, Madder H, Moir I, Moroney R, Quan TP, et al. A Candida auris outbreak and its control in an intensive care setting. N Engl J Med. 2018;379:1322–31. DOIPubMedGoogle Scholar
- Center for Disease Control and Prevention. Screening for Candida auris colonization [cited 2022 Jun 8]. https://www.cdc.gov/fungal/candida-auris/c-auris-screening.html
- Sexton DJ, Kordalewska M, Bentz ML, Welsh RM, Perlin DS, Litvintseva AP. Direct detection of emergent fungal pathogen Candida auris in clinical skin swabs by SYBR green-based quantitative PCR assay. J Clin Microbiol. 2018;56:1–6. DOIPubMedGoogle Scholar
- Moema I, Ismail H, van Schalkwyk E, Shuping L, Govender N. Outbreak of culture-confirmed Candida auris bloodstream infection in the neonatal unit of a public-sector hospital, South Africa, July through September 2017. FEAD: the Field Epidemiology Abstract Database. 2017 [cited 2022 Jun 25]. https://www.tephinet.org/learning/fead/outbreak-of-culture-confirmed-candida-auris-bloodstream-infection-in-the-neonatal-unit
- Sexton DJ, Bentz ML, Welsh RM, Derado G, Furin W, Rose LJ, et al. Positive correlation between Candida auris skin-colonization burden and environmental contamination at a ventilator-capable skilled nursing facility in Chicago. Clin Infect Dis. 2021;73:1142–8. DOIPubMedGoogle Scholar
- Huang X, Hurabielle C, Drummond RA, Bouladoux N, Desai JV, Sim CK, et al. Murine model of colonization with fungal pathogen Candida auris to explore skin tropism, host risk factors and therapeutic strategies. Cell Host Microbe. 2021;29:210–221.e6. DOIPubMedGoogle Scholar
- Ghannoum M, Herrada J, McCormick TS, Long L. A novel transdermal application for clearing skin colonization by Candida auris. Antimicrob Agents Chemother. 2023;95:1–6.PubMedGoogle Scholar
- Proctor DM, Dangana T, Sexton DJ, Fukuda C, Yelin RD, Stanley M, et al.; NISC Comparative Sequencing Program. Integrated genomic, epidemiologic investigation of Candida auris skin colonization in a skilled nursing facility. Nat Med. 2021;27:1401–9. DOIPubMedGoogle Scholar
- Ahmad A, Spencer JE, Lockhart SR, Singleton S, Petway DJ, Bagarozzi DA Jr, et al. A high-throughput and rapid method for accurate identification of emerging multidrug-resistant Candida auris. Mycoses. 2019;62:513–8. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: August 08, 2023
Table of Contents – Volume 29, Number 9—September 2023
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Liliwe Shuping, Centre for Healthcare-Associated Infections, Antimicrobial Resistance and Mycoses, National Institute for Communicable Diseases, National Health Laboratory Service, 1 Modderfontein Rd, Sandringham, Johannesburg, 2131, South Africa
Top