Volume 25, Number 11—November 2019
Dispatch
Secondary Autochthonous Outbreak of Chikungunya, Southern Italy, 2017
Abstract
In 2017, a chikungunya outbreak in central Italy later evolved into a secondary cluster in southern Italy, providing evidence of disease emergence in new areas. Officials have taken action to raise awareness among clinicians and the general population, increase timely case detection, reduce mosquito breeding sites, and promote mosquito bite prevention.
In 2007 (1) and 2017 (2), local outbreaks of human chikungunya infection occurred in Italy; both outbreaks were caused by the East/Central/South African strain of chikungunya virus (CHIKV). Both outbreaks were sustained by the invasive mosquito Aedes albopictus, largely established in Italy and other countries in southern Europe (3). In 2017, France and Italy reported local transmission of CHIKV (2,4). However, in France, the number of cases was limited; whereas in Italy, 499 probable and confirmed cases of locally acquired CHIKV infection occurred, of which 270 were laboratory confirmed as per the European Union (EU) case definition of June 22, 2018 (https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32018D0945&from=EN#page=13).
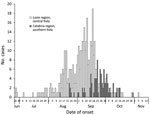
After local CHIKV transmission was confirmed in the seaside city of Anzio (Lazio region, central Italy) in 2017, the outbreak spread within the region, including in the city of Rome (5–7). The beginning of the outbreak was traced back to June 2017 (Figure 1). Subsequently, an outbreak developed in Guardavalle Marina, a small village of 2,346 inhabitants in the Calabria region of southern Italy, causing 100 probable/confirmed cases (Figures 1, 2).
In August 2017, a patient from Anzio arrived in Guardavalle Marina the day before onset of symptoms that met the clinical criteria of the EU case definition for chikungunya (suspected case); subsequently, more cases in the village were reported. For most case-patients, the clinical course of the disease was fairly mild. All patients with confirmed/probable cases reported fever, and 99% reported severe and persistent joint pain, which seemed to be the most indicative symptom of chikungunya (Appendix Table 2). Phylogenetic analysis of isolates from patients with confirmed cases and from mosquito pools showed that the virus strains from Lazio and Calabria were similar to the East/Central/South African strains detected in Pakistan and India (2,8). Neither strain contained the A226V mutation that was detected in the strain responsible for the 2007 outbreak in Italy (1).
The epidemiologic and microbiological evidence (Appendix) supports the hypothesis that the Guardavalle Marina outbreak originated from Lazio rather than from an independent introduction. The overall clinically observed attack rate in Guardavalle Marina was 4.3%, similar to the 5.4% rate reported during the 2007 outbreak in Castiglione di Cervia but much lower than the 34% rate reported in La Réunion (9) or the high attack rates typically reported by other affected tropical countries (10). The duration of the Guardavalle Marina outbreak (2 months) was also closer to the duration of the outbreak in Castiglione di Cervia (July–September 2007) than to the duration of the outbreak in La Réunion (March 2005–April 2006) (11).
Clinically observed attack rates progressively increased with patient age (Appendix Table 1). This pattern was also observed during the 2007 outbreak in Italy (1) and was mainly attributed to older age being a proxy for specific behavior linked to higher exposure to bites from Ae. albopictus mosquitoes (12). We cannot exclude underestimation of the observed attack rate in Guardavalle Marina, even though extensive door-to-door case finding was feasible and performed, given the small size of the village.
Notwithstanding the lack of the A226V mutation, the 2017 strain was introduced and rapidly spread with evidence of disease emergence in new areas. Statistically significant case clustering was confirmed by spatiotemporal data analysis in Guardavalle Marina (Appendix Figure 2), and Ae. albopictus mosquito vector competence for the 2017 strain was recently found to be comparable to competence for the 2007 mutated strain (13).
Delayed clinical detection of cases, possibly resulting from lack of CHIKV infection awareness among clinicians (14), and hence delayed testing for laboratory confirmation, could explain the size and extension of the 2017 outbreak. The fact that the outbreak was contained in a relatively short time after detection could be the result of the combination of targeted vector control interventions (Appendix), cooling temperatures, and increased rainfall during October–November 2017.
Since 2011, Italy has had a yearly updated plan for the surveillance and control of human infections caused by CHIKV; the plan includes designated reference laboratories, vector control, and blood/transplant safety measures (Appendix). After the 2017 outbreak, a “presumed local cluster” was defined as occurring when local transmission of CHIKV is suspected for >2 cases, of which only 1 case needs to be laboratory confirmed. It is sufficient for the second case to be suspected on clinical and epidemiologic grounds pending laboratory confirmation. This new definition, aimed at triggering more timely blood/transplant safety and outbreak response measures, was successfully implemented in 2018. Actions to raise awareness among clinicians and the general population are being designed as part of a joint effort of animal and human public health institutions and universities coordinated by the Italy Ministry of Health. These actions are aimed at increasing timely case detection, reducing the number of mosquito breeding sites, and promoting individual prevention of mosquito bites.
Dr. Riccardo is an infectious disease specialist and epidemiologist working in the Department of Infectious Diseases of the National Institute of Health in Rome (Istituto Superiore di Sanità). Her research interests include emerging and vectorborne diseases.
Acknowledgment
We acknowledge the work and contribution of Giuseppe Ussia and Felice Valente in the detection and control of the outbreak described and all general practitioners and pediatricians involved in the detection and management of cases: Pietro Spadola, Antonio Tedesco, Giuseppe Montepaone, Antonio Rosario Lioi, Teresa Tropea, Serafina Gallo, Enzo Valente. We also acknowledge the work of Guido Sansotta, Alberto Meleca, Francesco Giancotti, Giada Rossini, Caterina Vocale, Paolo Gaibani, Simone Lanini, Alessia Mammone, and Virginia Di Bari.
References
- Rezza G, Nicoletti L, Angelini R, Romi R, Finarelli AC, Panning M, et al.; CHIKV study group. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370:1840–6. DOIPubMedGoogle Scholar
- Venturi G, Di Luca M, Fortuna C, Remoli ME, Riccardo F, Severini F, et al. Detection of a chikungunya outbreak in central Italy, August to September 2017. Euro Surveill. 2017;22:pii=17-00646.
- European Centre for Disease Prevention and Control. Aedes albopictus–current known distribution in Europe, April 2017 [cited 2019 Jan 8]. https://ecdc.europa.eu/en/publications-data/aedes-albopictus-current-known-distribution-europe-april-2017
- Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Euro Surveill. 2017;22:pii=17-00647
- European Centre for Disease Prevention and Control. Rapid risk assessment. Clusters of autochthonous chikungunya cases in Italy: first update 9 October 2017 [cited 2019 Jan 8]. https://ecdc.europa.eu/sites/portal/files/documents/RRA-chikungunya-Italy-update-9-Oct-2017.pdf
- Manica M, Guzzetta G, Poletti P, Filipponi F, Solimini A, Caputo B, et al. Transmission dynamics of the ongoing chikungunya outbreak in central Italy: from coastal areas to the metropolitan city of Rome, summer 2017. Euro Surveill. 2017;22:pii=17-00685.
- Vairo F, Mammone A, Lanini S, Nicastri E, Castilletti C, Carletti F, et al.; Chikungunya Lazio Outbreak Group. Local transmission of chikungunya in Rome and the Lazio region, Italy. PLoS One. 2018;13:
e0208896 . DOIPubMedGoogle Scholar - Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak chikungunya virus belongs to an emerging Aedes albopictus adapted virus cluster introduced from the Indian subcontinent [cited 2019 Jan 7]. https://academic.oup.com/ofid/advance-article/doi/10.1093/ofid/ofy321/5239584
- Larrieu S, Balleydier E, Renault P, Baville M, Filleul L. Epidemiological surveillance of chikungunya on Reunion Island between 2005 and 2011 [in French]. Med Trop (Mars). 2012;72:38–42.
- Staples JE, Breiman RF, Powers AM. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin Infect Dis. 2009;49:942–8. DOIPubMedGoogle Scholar
- Josseran L, Paquet C, Zehgnoun A, Caillere N, Le Tertre A, Solet JL, et al. Chikungunya disease outbreak, Reunion Island. Emerg Infect Dis. 2006;12:1994–5. DOIPubMedGoogle Scholar
- Moro ML, Gagliotti C, Silvi G, Angelini R, Sambri V, Rezza G, et al.; Chikungunya Study Group. Chikungunya virus in North-Eastern Italy: a seroprevalence survey. Am J Trop Med Hyg. 2010;82:508–11. DOIPubMedGoogle Scholar
- Fortuna C, Toma L, Remoli ME, Amendola A, Severini F, Boccolini D, et al. Vector competence of Aedes albopictus for the Indian Ocean lineage (IOL) chikungunya viruses of the 2007 and 2017 outbreaks in Italy: a comparison between strains with and without the E1:A226V mutation. Euro Surveill. 2018;23:1800246.
- Russo G, Caputo B, Di Lascio A, Gatto G, Solimini AG. Awareness towards chikungunya virus infection risk by general practitioners in Rome: a questionnaire based survey before the 2017 outbreak. Infectious Diseases and Tropical Medicine. 2018;4:
e451 .
Figures
Cite This ArticleOriginal Publication Date: September 26, 2019
1These authors contributed equally to this article.
Table of Contents – Volume 25, Number 11—November 2019
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Flavia Riccardo, Istituto Superiore di Sanità, Dipartimento Malattie Infettive, Viale Regina Elena 299, 00161 Rome, Italy
Top