Volume 26, Number 10—October 2020
Research Letter
Effect of COVID-19 on Tuberculosis Notification, South Korea
Abstract
After South Korea raised its infectious disease alert to the highest level in response to coronavirus disease emergence, tuberculosis notification during the first 18 weeks of 2020 decreased significantly from the same period for each year during 2015–2019. Adequate measures to diagnose, control, and prevent tuberculosis need to be maintained.
The first case of coronavirus disease (COVID-19) in South Korea was identified on January 20, 2020, and an outbreak from a church hastened widespread transmission throughout the country (1). On February 23, the government of South Korea raised the country’s infectious disease alert to the highest level and initiated vigorous infection control measures: establishing widespread diagnostic capacity, initiating local contact tracing, mandating physical distancing, and redesigning triage and treatment systems (2). While this alert level remains in effect, such measures could negatively affect other communicable diseases, such as tuberculosis (TB) (3). To investigate the effect of COVID-19 on TB diagnoses, we traced the number of notified TB cases in South Korea before and after the COVID-19 outbreak started and compared them with previous years, during which the burden of TB has been at an intermediate level.
We gathered the weekly number of newly notified TB cases for 2015–2020 from the Public Health Weekly Report released by the Korea Centers for Disease Control and Prevention. In South Korea, physicians and healthcare workers are required to report confirmed or clinically diagnosed TB to health authorities within 24 hours, irrespective of any previous history of TB treatment (4). The Public Health Weekly Report publishes the number of notified TB cases by province every week (1). In addition, the number of confirmed COVID-19 cases is posted daily on the Korea Centers for Disease Control and Prevention website (1).
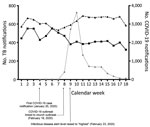
We calculated the mean number of weekly TB notifications from the 1st through the 18th week of each year from 2015 through 2019. We also collected the weekly number of notified TB cases during the same period in 2020. We compared the number of cases before and after the highest alert level was declared (weeks 1–8 [before the COVID-19 outbreak began] and weeks 9–18 [after the COVID-19 outbreak began]). We estimated the change in the number of notified TB cases in 2020 after the COVID-19 outbreak started by comparing the latest numbers with those from previous years using a Bayesian structural time-series model (5). We used R statistical software version 4.0.2 (https://www.r-project.org) for all statistical analyses.
During 2015–2019, a mean number of 594 TB cases were notified weekly during weeks 1–8 and a mean number of 655 TB cases were notified weekly during weeks 9–18. In 2020, a mean of 498 TB cases were notified each week during weeks 1–8; the mean number of notifications during weeks 9–18 decreased to 390 cases/week. After COVID-19 began, TB notification decreased by 24% (121 cases/week; p<0.01 from the predicted number in 2020 based on a Bayesian structural time-series model) (Figure). In Daegu and Gyeongbuk Provinces, the epicenter of COVID-19 in South Korea, TB notification decreased by 23% (14 cases/week; p = 0.003). In other provinces, patterns were similar; TB notification decreased by 25% (112 cases/week; p = 0.001) after COVID-19 began (Table).
Our analysis demonstrated that the COVID-19 pandemic led to a decrease in TB notification in South Korea and that this reduction was not confined to the Daegu and Gyeongbuk Province areas. Although the number of TB cases in South Korea has decreased steadily since 2010 (6), the 24% decrease in TB notification after COVID-19 began is larger than that predicted by our time-series model.
The reduced number of TB notifications could reflect decreased transmission associated with physical distancing and the increased use of face masks. Recent analysis proposed that physical distancing could decrease transmission of TB by 10% in high TB burden countries (7). However, the 24% reduction in South Korea, which has an intermediate burden of TB, suggests the additional contribution of other factors. First, during the COVID-19 outbreak, interventions such as TB contact investigation and preventive therapy may have been deprioritized and delayed (3). Second, patients with newly developed respiratory symptoms could not visit chest clinics easily because those patients were redirected to COVID-19 screening clinics to prevent in-hospital transmission (8).
The negative effect of the COVID-19 outbreak on TB has not been confined to diagnosis. In South Korea, outpatient clinics and emergency departments have been temporarily closed after patients visiting the facility have been identified as having COVID-19 (9). Negative-pressure units also have been prioritized for COVID-19 patients (2). Overall healthcare use worsens during outbreaks of communicable diseases, as demonstrated by the 10%–23% decrease in emergency department visits, even for life-threatening conditions, after COVID-19 began, as reported in the United States (10).
In summary, we found that TB notifications decreased significantly with the surge of COVID-19 in South Korea. Adequate measures to diagnose, control, and prevent TB, a much older and more burdensome infectious killer than COVID-19, need to be maintained during this pandemic.
Dr. Kwak is an assistant professor and a chest physician at Seoul National University Hospital. His research interests focus on nontuberculous mycobacterial pulmonary disease and pulmonary tuberculosis.
References
- Korea Centers for Disease Control and Prevention. Public Health Weekly Report [in Korean] [cited 2020 Jul 1]. https://www.cdc.go.kr/board/board.es?mid=a30501000000&bid=0031&cg_code=C04
- Oh J, Lee J-K, Schwarz D, Ratcliffe HL, Markuns JF, Hirschhorn LR. National response to covid-19 in the Republic of Korea and lessons learned for other countries. Health Syst Reform. 2020;6:
e1753464 . DOIPubMedGoogle Scholar - Pai M. COVID-19 coronavirus and tuberculosis: we need a damage control plan. Forbes. 2020 Mar 17 [cited 2020 Jul 1]. https://www.forbes.com/sites/madhukarpai/2020/03/17/covid-19-and-tuberculosis-we-need-a-damage-control-plan/#f72dd45295ca
- Kim JH, Yim J-J. Achievements in and challenges of tuberculosis control in South Korea. Emerg Infect Dis. 2015;21:1913–20. DOIPubMedGoogle Scholar
- Brodersen KH, Gallusser F, Koehler J, Remy N, Scott SL. Inferring causal impact using Bayesian structural time-series models. Ann Appl Stat. 2015;9:247–74. DOIGoogle Scholar
- Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis in Korea. 2019 [in Korean] [cited 2020 Jul 14]. http://tbzero.cdc.go.kr/tbzero/main.do?pageEvent=N
- Stop TB. Partnership. The potential impact of the covid-19 response on tuberculosis in high-burden countries: modelling analysis [cited 2020 Jul 1]. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf
- Ministry of Health and Welfare. Republic of Korea. Guidelines for the operation of screening center for COVID-19. 8th version [in Korean] [cited 2020 Jul 1]. http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=24
- Lee H, Heo JW, Kim SW, Lee J, Choi JH. A lesson from temporary closing of a single university-affiliated hospital owing to in-hospital transmission of coronavirus disease 2019. J Korean Med Sci. 2020;35:
e145 . DOIPubMedGoogle Scholar - Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:795–800. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleOriginal Publication Date: July 16, 2020
Table of Contents – Volume 26, Number 10—October 2020
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Jae-Joon Yim, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, 101 Daehak-Ro, Jongno-Gu, Seoul 110-744, South Korea
Top