Volume 29, Number 8—August 2023
Synopsis
Outbreak of NDM-1– and OXA-181–Producing Klebsiella pneumoniae Bloodstream Infections in a Neonatal Unit, South Africa
Abstract
After an increase in carbapenem-resistant Klebsiella pneumoniae (CRKP) bloodstream infections and associated deaths in the neonatal unit of a South Africa hospital, we conducted an outbreak investigation during October 2019–February 2020 and cross-sectional follow-up during March 2020–May 2021. We used genomic and epidemiologic data to reconstruct transmission networks of outbreak-related clones. We documented 31 cases of culture-confirmed CRKP infection and 14 deaths. Two outbreak-related clones (blaNDM-1 sequence type [ST] 152 [n = 16] and blaOXA-181 ST307 [n = 6]) cocirculated. The major clone blaNDM-1 ST152 accounted for 9/14 (64%) deaths. Transmission network analysis identified possible index cases of blaOXA-181 ST307 in October 2019 and blaNDM-1 ST152 in November 2019. During the follow-up period, 11 new cases of CRKP infection were diagnosed; we did not perform genomic analysis. Sustained infection prevention and control measures, adequate staffing, adhering to bed occupancy limits, and antimicrobial stewardship are key interventions to control such outbreaks.
Carbapenem-resistant Enterobacterales (CRE) are classified as critical priority bacterial pathogens by the World Health Organization (1). Klebsiella pneumoniae is a major cause of neonatal infections in low- and middle-income countries (2,3). In a national population-level analysis, K. pneumoniae accounted for 26% of invasive neonatal infections in South Africa during 2014–2019 (4). Resistance mechanisms to carbapenems include enzymatic inactivation, changes to outer-membrane permeability, and efflux pump upregulation (5). Several outbreaks of K. pneumoniae infection in neonatal units have been investigated in South Africa since 1992 (6–11). Some of those studies used molecular typing methods, such as multilocus sequence typing and pulsed-field gel electrophoresis (PFGE), that lack sufficient resolution to distinguish between clonal strains (8–12). Whole-genome sequencing (WGS) is a powerful tool to investigate healthcare-associated pathogens such as K. pneumoniae and has been widely used in combination with epidemiologic information to track outbreaks and transmission routes of pathogens (13–17).
In December 2019, the National Institute for Communicable Diseases (NICD) in South Africa was notified of 8 cases of culture-confirmed carbapenem-resistant K. pneumoniae (CRKP) bloodstream infections in a neonatal unit at a provincial tertiary hospital. The outbreak began with 4 cases reported in October 2019. The objectives of this investigation were to verify the existence of an outbreak; describe the antimicrobial susceptibility profiles, resistance mechanisms, and transmission dynamics of CRKP clones in circulation; and monitor the incidence of CRKP infections within 1 year of instituting outbreak interventions.
Hospital Setting and Surveillance
Tembisa Provincial Tertiary Hospital is located in the Tembisa township in Gauteng Province, South Africa; the township has a population size of 2.5 million. The hospital also serves the communities of Midrand and Diepsloot and as a referral site for 20 clinics in the surrounding area, spanning 3 municipalities (the cities of Johannesburg, Ekurhuleni, and Tshwane). Annually, the hospital sees >280,000 patients. The hospital facility has 840 beds in total, 704 for adults, 71 for newborn babies, and 64 for pediatric patients; the average daily admission is 150 patients. The hospital’s neonatal unit consists of wards A and B. Neonates are assigned to a section within a ward depending on age and the acuity of their condition at admission. Ward A has high-care (A1), low-care (A2), and isolation rooms; the approved bed capacity is 40. Ward B consists of a kangaroo mother care section (designed to increase skin-to-skin contact between mother and infant for preterm or low birthweight infants), a neonatal intensive care unit, a low-care unit, and a pediatric intensive care unit that is separated from the other rooms by a door. Ward B has a total of 31 beds. The intended medical staff complement during a day shift in ward A was 8 doctors, with an intended bed-to-doctor ratio of 5:1 and an intended bed-to-nurse ratio of 3:1. One medical officer was usually on night call for all the neonatal wards. Ward B had 3 doctors and 4 nurses, with an overall bed-to-staff ratio of 4.4:1.
Coincidentally, enhanced surveillance for neonatal infections as part of the Baby GERMS-SA study was conducted at this hospital during October 1, 2019–September 30, 2020 (18). In brief, neonates with culture-confirmed bloodstream infections or meningitis were enrolled into the surveillance program if they met the case definition (i.e., a neonate <28 days of age from whom a pathogen was isolated from blood or cerebrospinal fluid). The diagnostic laboratory submitted the corresponding bacterial and fungal isolates to the NICD for further characterization. Demographic, clinical, and outcome data were retrospectively abstracted from their imaged medical records. In addition, admissions and patient bed-days were recorded by month for the neonatal unit.
Outbreak Investigation
A multidisciplinary investigation team consisting of members of the NICD, Infection Control Service Laboratory (National Health Laboratory Service), the Gauteng Provincial Department of Health, and the National Department of Health was assembled in January 2020. To estimate baseline rates of bloodstream infections, we obtained a line list from the NICD surveillance data warehouse for infants <6 months of age admitted to Tembisa Provincial Tertiary Hospital with blood cultures positive for any bacterial or fungal organism during January 2017–September 2019. We excluded organisms considered commensals by the US Centers for Disease Control and Prevention National Healthcare Safety Network (19). We regarded blood cultures with the same organism isolated within 21 days of the first positive culture as duplicates and excluded those. We defined an outbreak as an increase of >100% in the number of observed cases of CRKP infection in a month above the expected (average) number in the preceding 2 months. On March 11, 2020, before the initial investigation closeout, the World Health Organization declared the global COVID-19 pandemic (20). We calculated monthly bloodstream infection rates during the follow-up period, March 2020–May 2021, using the same methods used in the initial outbreak investigation.
External Infection Prevention and Control Audit Process
During the initial investigation, we conducted an external infection prevention and control (IPC) audit in January 2020 using the National Department of Health standardized Infection Control Assessment Tool (21). We compiled recommendations for immediate, mid-term, and long-term interventions. A similar internal audit by the hospital response team was conducted in August 2020 to monitor improvements in adherence to IPC measures. Specific IPC measures had been implemented early after the observed increase in the number of cases. For instance, all colonized and infected babies were cohorted or isolated in separate sections of the ward. Additional cleaning of the unit was conducted several times beginning in November 2019. Hand hygiene was monitored for both staff and parents entering the unit. When the neonatal unit reached 100% bed capacity, maternity cases were rerouted to other facilities, although this intervention could not be sustained during the COVID-19 pandemic.
Cases and Isolates
We defined a case as culture-confirmed bloodstream infection caused by K. pneumoniae resistant to any carbapenem (i.e., meropenem, imipenem, doripenem, or ertapenem) in an infant <6 months of age. The case definition was not restricted to neonates <28 days of age because babies who stayed in hospital beyond the neonatal period remained at risk for infection. We analyzed all isolates submitted to NICD from this hospital during October 1, 2019–February 29, 2020, including those submitted for Baby GERMS-SA surveillance. The hospital provided monthly infection reports to NICD, listing cases of CRKP infection with dates of birth, birthweights, dates of specimen collection, and outcome information. We conducted the follow-up analysis in May 2021, 18 months after the outbreak started in October 2019.
Microbiological Analysis
We confirmed species-level identification using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (Bruker Daltonics, https://www.bruker.com) and performed antimicrobial susceptibility testing using the MicroScan WalkAway 96-plus system with the NM44 card (Siemens Healthineers, https://www.siemens-healthineers.com). We interpreted MICs for the tested antimicrobial agents according to Clinical and Laboratory Standards Institute guidelines and defined multidrug-resistant isolates as those with nonsusceptibility to >1 agent in >3 antimicrobial classes (22). We screened for carbapenemase genes and strain relatedness using real-time multiplex PCR and PFGE and performed WGS to determine sequence types, identify acquired antimicrobial resistance genes, and confirm presence of plasmid replicons, O antigen locus types, and K locus types. We compared core genome single-nucleotide polymorphism (SNP) distances and epidemiologic information to investigate the transmission events of CRKP in the neonatal unit (Appendix).
Baseline, Outbreak, and Follow-Up Periods
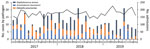
During January 2017–September 2019, a total of 1,771 positive blood cultures were reported from infants <6 months of age at the hospital. Of those, 864 (49%) blood cultures yielded probable pathogenic organisms; 724 were in neonatal wards A and B. We excluded 144 duplicates from the analysis. Of the remaining 580 isolates, 428 were from patients with single-isolate bloodstream infection episodes and were included in the analysis. K. pneumoniae accounted for 29% (122/428) of cases, Staphylococcus aureus 36% (153/428), and Acinetobacter baumannii 27% (116/428). Of the 122 cases of K. pneumoniae isolated during the January 2017–September 2019 baseline period, 8% (10/122) were CRKP; 5 of those cases were diagnosed in January 2019 (Figure 1).
The number of CRKP bloodstream infection cases increased during October 1, 2019–February 29, 2020; a total of 31 cases and 15 deaths were reported. Most cases (n = 14) were reported in December 2019; in the preceding 2 months only 3 non-CRKP cases were diagnosed (average 1.5 cases/month) (Figure 2).
During the follow-up period (March 2020–May 2021), 299 positive blood cultures with probable pathogenic organisms were obtained from infants admitted to the neonatal unit (wards A and B). K. pneumoniae accounted for 38 of those episodes (13%); of those, 29% (n = 11) isolates were carbapenem-resistant (Appendix).
External IPC Audit Findings and Internal Follow-Up Audit
The initial external IPC auditors found that neonatal unit ward A exceeded the approved bed capacity by 60% (64 admissions in a ward with 40 approved beds); ward A had 13 nurses per shift and a bed-to-nurse ratio of 5:1. Occupancy increased to 180% above the approved capacity during the internal audit in August 2020. Attrition occurred at a rate of 16 nurses and 13 clinical staff over a period of 7 months. Adherence to hand hygiene was 95% during the external audit and 100% during the follow-up internal audit. Hand hygiene adherence remained at >96% a year later in May 2021, maintained through a peer-monitoring system. Liquid hand soap with an antimicrobial agent, alcohol-based antiseptic, and hand lotions (aqueous cream) were initially not available for staff, but availability improved on follow-up. Alcohol-based antiseptic dispensers were available at each bed during the follow-up audit. Handwashing supplies were ordered, and stock levels were monitored. Elbow-operated taps were installed to improve quality of hand hygiene practices. Unannounced IPC audits were performed, but no direct observations were reported. The overall score for sterilizing and disinfecting instruments improved from 27% to 47% in August 2020. Policies or standard operating procedures (SOPs) were subsequently developed, and staff members signed to demonstrate their understanding of SOPs. The unit had no designated area for mixing standard intravenous fluids because of infrastructural challenges, single-dose vials were not used, and no SOP for multidose vials was in place in the ward (Appendix Table). Most external audit recommendations were implemented. For example, an integrated IPC and occupational health and safety team was established to maximize human resource capacity and budget allocations and to strengthen infection surveillance. However, some crucial initial IPC audit recommendations could not be sustained because of COVID-19 demands (e.g., diverting patients to neighboring hospitals when ward capacity was reached and converting the milk room into a kangaroo mother care unit). Although an antimicrobial stewardship committee was established, implementing its recommendations was delayed because attention and resources were diverted to the COVID-19 response.
Isolates and Cases
During October 2019–February 2020, a total of 31 laboratory-confirmed cases of CRKP bloodstream infections were reported in the neonatal unit. Of those, we did not have isolates for 2 cases (Figure 3), but laboratory reports indicated that these isolates were resistant to ertapenem, imipenem, and meropenem. The NICD reference laboratory received 34 isolates for the remaining 29 cases. Of those, 2 cases had 3 isolates each and 1 case had 2 isolates. The first isolate (i.e., the isolate with earliest specimen collection date) per case from 29 cases was selected for molecular characterization. Twenty-seven isolates were confirmed as K. pneumoniae subspecies pneumoniae; antimicrobial susceptibility profiling and genomic characterization was performed. We excluded 2 isolates identified as Pseudomonas aeruginosa that were likely contaminated during shipping.
Antimicrobial Susceptibility
All isolates were multidrug-resistant. In total, 89% (24/27) of the isolates were resistant to ertapenem and 81% (22/27) were resistant to meropenem (Figure 3).
Genomic Characterization
We identified 3 clonal clusters consisting of 6 sequence types from 27 isolates by using core genome maximum-likelihood phylogeny (Appendix Figure 1). Sequence type (ST) 152 accounted for 59% (16/27) of the cases, followed by ST307 (6/27; 22%) and ST17 (2/27; 7%); ST25, ST45, and ST297 each accounted for a single case (1/27; 4%). We found that 94% (26/27) of the isolates carried carbapenemase genes. All isolates within ST152 clone harbored the blaNDM-1 gene and contained ColRNAI, IncFIB(K), IncFIB(pB171), and IncFII(Yp) plasmid incompatibility groups. Further analysis revealed that the blaNDM-1 gene was carried on the Escherichia coli B171 plasmid pB171 (accession no. AB024946). Phenotypic resistance to third and fourth generation cephalosporins was confirmed by the presence of extended-spectrum β-lactamases, such as blaCTX-M-15 and other β-lactamase genes (blaTEM-1 and blaSHV-1) (Appendix Figure 1).
The gene blaOXA-181 was present in all isolates belonging to ST307. Three isolates carrying the blaOXA-181 gene coharbored the blaOXA-48 gene. All isolates within blaOXA-181 ST307 clone shared ColKP3, IncFIB(Mar), and IncX3 plasmid incompatibility groups. Plasmid analysis showed that blaOXA-181 gene in ST307 clone isolates was carried on K. pneumoniae KP3 plasmid KP3-A (accession no. JN205800) (Appendix Figure 1).
Clinical Characteristics of 26 WGS-Confirmed Cases of CRKP
Of the 26 WGS-confirmed cases of CRKP, 67% (18/26) of the infants were boys; median age was 7 days (interquartile range 3–17 days). Birthweights ranged from 760 to 3,200 g; the median weight was 1,100 g (interquartile range 970–1595 g). Four of the 26 infants required resuscitation at birth. Invasive devices were inserted in all infants. Two infants had a record of underlying abnormalities (congenital anemia and neonatal seizures). Just over half (54% [14/26]) of infants died in hospital. Of these, 64% (9/14) had cultured isolates belonging to the ST152 clone (Table).
Genomic and Epidemiologic Links among Outbreak-Associated Isolates
The first case (Pt1) of CRKP BSI blaOXA-181 ST307 clone was confirmed on October 10, 2019 in ward A. The blaOXA-181 ST307 was responsible for 4 more cases (2 each in wards A and B) in late November and during the first week of December 2019. The last case belonging to blaOXA-181 ST307 clone was identified in January 2020. The transmission network revealed that Pt1 was a possible index case. Although this patient was later transferred to an academic hospital for further treatment, this clone continued to disseminate within the neonatal unit. Five more cases were detected with the transmission stemming from the intermediate host with SNP differences of <10 among the clonal isolates (Figure 4, panel A).
The first case-patient (Pt4) of the major outbreak-related blaNDM-1 ST152 clone was diagnosed on November 15, 2019, in ward A of the neonatal unit, followed by another case (Pt7) 15 days later in ward A. During December 11, 2019–February 2, 2020, a total of 14 more cases were isolated in the neonatal unit. Isolates from Pt14 and Pt17 were not considered part of the outbreak because they had >30 SNPs compared to other isolates. No further cases caused by the blaNDM-1 ST152 clone were diagnosed after February 2020. Transmission network analysis identified Pt4 as the index case for the ST152 clone outbreak. However, Pt4 died on November 16, 2019, ten days before Pt7 was admitted, suggesting the role of an intermediate host or environmental source in the dissemination of blaNDM-1 ST152 clone in the neonatal unit. Pt8’s infection was diagnosed 2 days after the diagnosis of Pt7. Pt8 died a day after diagnosis. No further transmission from Pt7 or Pt8 to other patients could be established. Nine patients (Pt12–Pt19 and Pt22) in whom transmission stemmed directly from Pt4 were potentially infected through an intermediate source. Further dissemination of the ST152 clone was observed between Pt21, Pt23, and Pt26 in January 2020. These patients were admitted to ward A but moved between ward A and ward B. The transmission network revealed 2 possible events: first, from Pt21 to Pt24, who died a day after diagnosis; and second, that transmission occurred from Pt21 to Pt23, then from Pt23 to Pt26. However, Pt26 was admitted to ward A, 15 days after Pt23 was discharged from the hospital, suggesting the role of an intermediate in the spread of blaNDM-1 ST152 clone (Figure 4, panel B).
We describe the successful integration of genomic and epidemiologic data in tracking an outbreak of CRKP infections in the neonatal unit of a South Africa hospital. The number of CRKP bloodstream infections increased substantially in the neonatal unit beginning in October 2019. Two outbreak-related clones (blaNDM-1 ST152 and blaOXA-181 ST307) cocirculated. The major outbreak clone blaNDM-1 ST152 accounted for >60% of deaths. Fine transmission networks identified possible index cases of blaOXA-181 ST307 and blaNDM-1 ST152 clones. The spread and dissemination of these clones from patient to patient might have been enabled by healthcare workers or environmental or fomite contamination, resulting from breaches in IPC measures.
Reports of CRE infections in Africa have increased markedly; the most commonly reported carbapenemases are blaNDM-1 and blaOXA-48 and variants (23–27). In this study, K. pneumoniae carrying blaNDM-1, blaOXA-48, and blaOXA-181 were dominant in the neonatal unit, which was consistent with previous reports (23–27). The blaNDM gene was first described in South Africa in an Enterobacter cloacae strain in 2011 (28). Recent data from South Africa sentinel surveillance of CRE bloodstream infections have shown a change in the distribution of carbapenemase genes (29). Previously, blaNDM was the most commonly detected gene in Enterobacterales, followed by blaOXA-48 (25). However, beginning in 2016, blaOXA-48 and variants began to dominate, followed by blaNDM (29). This change is worrisome because blaOXA-48 and variants are more difficult to identify using phenotypic laboratory methods. Most outbreaks reported in South Africa are also associated with blaOXA-48 and variants (30–32). The emergence of blaNDM-1 K. pneumoniae as a cause of outbreaks is concerning because once inserted into drug-resistant plasmids, virulence determinants render these strains highly resistant, virulent, and easily transmissible regardless of the clone (33).
The first laboratory-confirmed outbreak of blaOXA-181 K. pneumoniae in South Africa was described in 2015 from a hematology unit in Cape Town (30). After that, Strydom et al. (31) identified K. pneumoniae superclone ST307 carrying blaOXA-181 on a self-transmissible plasmid IncX3 (p72_X3_OXA181) as the source of a CRKP outbreak that spread across multiple wards in a Pretoria hospital during September 2015–December 2016. Furthermore, blaOXA-181 was endemic among patients colonized with K. pneumoniae in a KwaZulu-Natal hospital intensive care unit, and the spread was enabled by plasmid replicon E. coli p010-B-OXA181 (32). A combination of genomic and epidemiologic data was used either to track outbreaks or reconstruct transmission events that occurred during an outbreak (14,16,34–36). In our study, blaNDM-1 and blaOXA-181 K. pneumoniae strains were responsible for outbreaks that occurred simultaneously in the neonatal unit. The resistant genes were spread by transmissible plasmids E. coli B171 plasmid pB171 (blaNDM-1) and K. pneumoniae KP3 plasmid KP3-A (blaOXA-181). A recent report describing an outbreak of CRKP bloodstream infections in a neonatal unit in another South Africa hospital showed that blaOXA-48 and variants K. pneumoniae were responsible for the outbreak (11). Although the main objectives of the outbreak investigation by Essel et al. (11) were to confirm the outbreak and assess the IPC program, the molecular typing technique used has low discriminatory power to distinguish genetically related isolates. Lowe et al. (37) documented the rapid spread of ST307 clone carrying blaOXA-181 in >40 hospitals across 3 provinces in South Africa, highlighting the critical need for more enhanced genomic surveillance of K. pneumoniae ST307 super clone in healthcare settings.
Given the rapid transfer and acquisition of endemic carbapenemase genes, IPC measures are critical to preventing and managing outbreaks. Both IPC audits flagged <50% adherence to instrument sterilization and disinfection procedures. Therefore, breaches in aseptic techniques during invasive medical device insertion or maintenance practices might have been involved in the causal pathway to neonatal bacteremia. Inadequate staffing, exceeded bed capacity, aging and undermaintained hospital infrastructure, and general lack of institutional support for IPC and antimicrobial stewardship initiatives also contribute to the spread of healthcare-associated infections (38). Dramowski et al. presented a framework for prevention of healthcare-associated infections in neonates and children, which highlighted the need for a nationally endorsed prevention strategy to ensure that children in South Africa receive safe and high-quality care (39).
The strength of this study was involvement of multiple stakeholders who enabled different segments of the outbreak investigation. Genomic and epidemiologic data were used to confirm the existence of the outbreak, identify the sources of the outbreak, and reconstruct probable transmission events. The first limitation of our study is that we conducted a search for cases of bloodstream infection among infants <6 months of age through a laboratory audit, but we did not extend this search to the rest of the hospital. Second, not all isolates from laboratory-confirmed CRKP cases were available for molecular characterization. Finally, genetic links among isolates from infected neonates and contaminated environment, fomites, or colonized healthcare workers could not be established because we did not perform contemporary environmental sampling or a colonization survey.
In conclusion, a combination of high-resolution WGS and epidemiologic data enabled a detailed description of this healthcare-associated infection outbreak in a neonatal unit and established transmission links. Continued monitoring of pathogens carrying endemic carbapenemases is necessary to prevent further reemergence of outbreaks. IPC measures complemented with adequate staffing levels, adherence to bed occupancy limits, improved neonatal unit infrastructure, and antimicrobial stewardship are key to sustainably reducing neonatal healthcare-associated infections.
Dr. Magobo is a medical scientist with experience in genomic epidemiology of bacterial and fungal pathogens causing healthcare-associated infections.
Acknowledgments
Members of Baby GERMS-SA: Nelesh P. Govender (principal investigator), Susan T. Meiring, Olga Perovic, Vanessa C. Quan, Anne von Gottberg, Linda de Gouveia, Cheryl Cohen, Angela Dramowski, Juliet Paxton, Danie Erwee, Camira Pillay, Rudzani C. Mashau, Rindidzani Magobo, Ntombi Dube, Relebohile Ramatsa, Melissa Ngubane, Bernard Motsetse, Lousia Phalatse, Tebogo Modiba, Dianette Pearce, Lesley Ingle, Zikhona Gabazana, Naseema Bulbulia, Patrick Pitjeng, Rosah Mabokachaba, Rotondwa Mudau, Rubeina Badat, Ruth Mogokotleng, Sabelle Jallow, Serisha Naicker, Siphiwe Kutta, Sydney Mogokotleng, Tsidiso Maphanga, Wilhelmina Strasheim (NICD, Johannesburg); site investigators: Cheryl Mackay (Dora Nginza Hospital, Eastern Cape), Mphekwa T Mailula (Mankweng Hospital, Limpopo), Rose Phayane (Tembisa Hospital, Gauteng), Constance Kapongo (Queen Nandi Regional Hospital, Kwa-Zulu-Natal), Omphile Mekgoe (Tshepong Hospital, North West), M. Terry (Rob Ferreira hospital, Mpumalanga).
This work was partly funded by the Bill and Melinda Gates Foundation (grant no. INV008112) (principal investigator N.P.G.).
References
- Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, et al.; WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18:318–27. DOIPubMedGoogle Scholar
- Okomo U, Akpalu ENK, Le Doare K, Roca A, Cousens S, Jarde A, et al. Aetiology of invasive bacterial infection and antimicrobial resistance in neonates in sub-Saharan Africa: a systematic review and meta-analysis in line with the STROBE-NI reporting guidelines. Lancet Infect Dis. 2019;19:1219–34. DOIPubMedGoogle Scholar
- Sands K, Carvalho MJ, Portal E, Thomson K, Dyer C, Akpulu C, et al.; BARNARDS Group. Characterization of antimicrobial-resistant Gram-negative bacteria that cause neonatal sepsis in seven low- and middle-income countries. Nat Microbiol. 2021;6:512–23. DOIPubMedGoogle Scholar
- Mashau RC, Meiring ST, Dramowski A, Magobo RE, Quan VC, Perovic O, et al.; Baby GERMS-SA. Culture-confirmed neonatal bloodstream infections and meningitis in South Africa, 2014-19: a cross-sectional study. Lancet Glob Health. 2022;10:e1170–8. DOIPubMedGoogle Scholar
- Queenan AM, Bush K. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev. 2007;20:440–58. DOIPubMedGoogle Scholar
- Coovadia YM, Johnson AP, Bhana RH, Hutchinson GR, George RC, Hafferjee IE. Multiresistant Klebsiella pneumoniae in a neonatal nursery: the importance of maintenance of infection control policies and procedures in the prevention of outbreaks. J Hosp Infect. 1992;22:197–205. DOIPubMedGoogle Scholar
- Pillay T, Pillay DG, Adhikari M, Sturm AW. Piperacillin/tazobactam in the treatment of Klebsiella pneumoniae infections in neonates. Am J Perinatol. 1998;15:47–51. DOIPubMedGoogle Scholar
- Gregersen N, Van Nierop W, Von Gottberg A, Duse A, Davies V, Cooper P. Klebsiella pneumoniae with extended spectrum beta-lactamase activity associated with a necrotizing enterocolitis outbreak. Pediatr Infect Dis J. 1999;18:963–7. DOIPubMedGoogle Scholar
- Cotton MF, Wasserman E, Pieper CH, Theron DC, van Tubbergh D, Campbell G, et al. Invasive disease due to extended spectrum beta-lactamase-producing Klebsiella pneumoniae in a neonatal unit: the possible role of cockroaches. J Hosp Infect. 2000;44:13–7. DOIPubMedGoogle Scholar
- Marais E, Moodley A, Govender N, Kularatne R, Thomas J, Duse A. Clusters of Klebsiella pneumoniae infection in neonatal intensive care units in Gauteng. S Afr Med J. 2006;96:813.PubMedGoogle Scholar
- Essel V, Tshabalala K, Ntshoe G, Mphaphuli E, Feller G, Shonhiwa AM, et al. A multisectoral investigation of a neonatal unit outbreak of Klebsiella pneumoniae bacteraemia at a regional hospital in Gauteng Province, South Africa. S Afr Med J. 2020;110:783–90. DOIPubMedGoogle Scholar
- Sabat AJ, Budimir A, Nashev D, Sá-Leão R, van Dijl J, Laurent F, et al.; ESCMID Study Group of Epidemiological Markers (ESGEM). Overview of molecular typing methods for outbreak detection and epidemiological surveillance. Euro Surveill. 2013;18:20380. DOIPubMedGoogle Scholar
- Smit PW, Stoesser N, Pol S, van Kleef E, Oonsivilai M, Tan P, et al. Transmission dynamics of hyper-endemic multi-drug resistant Klebsiella pneumoniae in a Southeast Asian neonatal unit: a longitudinal study with whole genome sequencing. Front Microbiol. 2018;9:1197. DOIPubMedGoogle Scholar
- Sui W, Zhou H, Du P, Wang L, Qin T, Wang M, et al. Whole genome sequence revealed the fine transmission map of carbapenem-resistant Klebsiella pneumonia isolates within a nosocomial outbreak. Antimicrob Resist Infect Control. 2018;7:70. DOIPubMedGoogle Scholar
- Chen D, Hu X, Chen F, Li H, Wang D, Li X, et al. Co-outbreak of multidrug resistance and a novel ST3006 Klebsiella pneumoniae in a neonatal intensive care unit: A retrospective study. Medicine (Baltimore). 2019;98:
e14285 . DOIPubMedGoogle Scholar - Wang Y, Luo C, Du P, Hu J, Zhao X, Mo D, et al. Genomic epidemiology of an outbreak of Klebsiella pneumoniae st471 producing extended-spectrum β-lactamases in a neonatal intensive care unit. Infect Drug Resist. 2020;13:1081–90. DOIPubMedGoogle Scholar
- Labi AK, Nielsen KL, Marvig RL, Bjerrum S, Enweronu-Laryea C, Bennedbæk M, et al. Oxacillinase-181 carbapenemase-producing Klebsiella pneumoniae in neonatal intensive care unit, Ghana, 2017–2019. Emerg Infect Dis. 2020;26:2235–8. DOIPubMedGoogle Scholar
- Meiring S, Mashau R, Magobo R, Perovic O, Quan V, Cohen C, et al. Study protocol for a population-based observational surveillance study of culture-confirmed neonatal bloodstream infections and meningitis in South Africa: Baby GERMS-SA. BMJ Open. 2022;12:
e049070 . DOIPubMedGoogle Scholar - Dudeck MA, Horan TC, Peterson KD, Allen-Bridson K, Morrell G, Anttila A, et al. National Healthcare Safety Network Report, data summary for 2011, device-associated module. 2013;41:286–300. PMID 23538117
- World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020 [cited 2021 Jun 30]. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- National Department of Health. Infection control assessment tool—September 2013. Pretoria: Government of South Africa.
- Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. DOIPubMedGoogle Scholar
- Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014;20:821–30. DOIPubMedGoogle Scholar
- Kieffer N, Nordmann P, Aires-de-Sousa M, Poirel L. High prevalence of carbapenemase-producing Enterobacteriaceae among hospitalized children in Luanda, Angola. Antimicrob Agents Chemother. 2016;60:6189–92. DOIPubMedGoogle Scholar
- Singh-Moodley A, Perovic O. Antimicrobial susceptibility testing in predicting the presence of carbapenemase genes in Enterobacteriaceae in South Africa. BMC Infect Dis. 2016;16:536. DOIPubMedGoogle Scholar
- Sangare SA, Rondinaud E, Maataoui N, Maiga AI, Guindo I, Maiga A, et al. Very high prevalence of extended-spectrum beta-lactamase-producing Enterobacteriaceae in bacteriemic patients hospitalized in teaching hospitals in Bamako, Mali. PLoS One. 2017;12:
e0172652 . DOIPubMedGoogle Scholar - Abderrahim A, Djahmi N, Pujol C, Nedjai S, Bentakouk MC, Kirane-Gacemi D, et al. First case of NDM-1-producing Klebsiella pneumoniae in Annaba University Hospital, Algeria. Microb Drug Resist. 2017;23:895–900. DOIPubMedGoogle Scholar
- Lowman W, Sriruttan C, Nana T, Bosman N, Duse A, Venturas J, et al. NDM-1 has arrived: first report of a carbapenem resistance mechanism in South Africa. S Afr Med J. 2011;101:873–5.PubMedGoogle Scholar
- Perovic O, Ismail H, Van Schalkwyk E, Lowman W, Prentice E, Senekal M, et al. Antimicrobial resistance surveillance in the South African private sector report for 2016. S Afr J Infect Dis. 2018;33:114–7. DOIGoogle Scholar
- Jacobson RK, Manesen MR, Moodley C, Smith M, Williams SG, Nicol MP, et al. Molecular characterisation and epidemiological investigation of an outbreak of blaOXA-181 carbapenemase-producing isolates of Klebsiella pneumoniae in South Africa. S Afr Med J. 2015;105:1030–5. DOIPubMedGoogle Scholar
- Strydom KA, Chen L, Kock MM, Stoltz AC, Peirano G, Nobrega DB, et al. Klebsiella pneumoniae ST307 with OXA-181: threat of a high-risk clone and promiscuous plasmid in a resource-constrained healthcare setting. J Antimicrob Chemother. 2020;75:896–902. DOIPubMedGoogle Scholar
- Madni O, Amoako DG, Abia ALK, Rout J, Essack SY. Genomic investigation of carbapenem-resistant Klebsiella pneumoniae colonization in an intensive care unit in South Africa. Genes (Basel). 2021;12:951. DOIPubMedGoogle Scholar
- Shankar C, Nabarro LEB, Muthuirulandi Sethuvel DP, Raj A, Devanga Ragupathi NK, Doss GP, et al. Draft genome of a hypervirulent Klebsiella quasipneumoniae subsp. similipneumoniae with novel sequence type ST2320 isolated from a chronic liver disease patient. J Glob Antimicrob Resist. 2017;9:30–1. DOIPubMedGoogle Scholar
- Onori R, Gaiarsa S, Comandatore F, Pongolini S, Brisse S, Colombo A, et al. Tracking nosocomial Klebsiella pneumoniae infections and outbreaks by whole-genome analysis: small-scale Italian scenario within a single hospital. J Clin Microbiol. 2015;53:2861–8. DOIPubMedGoogle Scholar
- Snitkin ES, Zelazny AM, Thomas PJ, Stock F, Henderson DK, Palmore TN, et al.; NISC Comparative Sequencing Program Group. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med. 2012;4:
148ra116 . DOIPubMedGoogle Scholar - Yang Y, Yang Y, Chen G, Lin M, Chen Y, He R, et al. Molecular characterization of carbapenem-resistant and virulent plasmids in Klebsiella pneumoniae from patients with bloodstream infections in China. Emerg Microbes Infect. 2021;10:700–9. DOIPubMedGoogle Scholar
- Lowe M, Kock MM, Coetzee J, Hoosien E, Peirano G, Strydom KA, et al. Klebsiella pneumoniae ST307 with blaOXA-181, South Africa, 2014-2016. Emerg Infect Dis. 2019;25:739–47. DOIPubMedGoogle Scholar
- Gill CJ, Mantaring JBV, Macleod WB, Mendoza M, Mendoza S, Huskins WC, et al. Impact of enhanced infection control at 2 neonatal intensive care units in the Philippines. Clin Infect Dis. 2009;48:13–21. DOIPubMedGoogle Scholar
- Dramowski A, Cotton MF, Whitelaw A. A framework for preventing healthcare-associated infection in neonates and children in South Africa. S Afr Med J. 2017;107:192–5. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleOriginal Publication Date: July 05, 2023
1Members of Baby GERMS-SA are listed at the end of this article.
Table of Contents – Volume 29, Number 8—August 2023
| EID Search Options |
|---|
|
|
|
|
|
|



Please use the form below to submit correspondence to the authors or contact them at the following address:
Nelesh P. Govender, National Institute for Communicable Diseases, Centre for Healthcare-Associated Infections, Antimicrobial Resistance and Mycoses, Private Bag X4, Sandringham, 2132, South Africa
Top