Volume 29, Number 8—August 2023
Dispatch
Increase of Severe Pulmonary Infections in Adults Caused by M1UK Streptococcus pyogenes, Central Scotland, UK
Abstract
We characterized the epidemiology, host–pathogen characteristics, and outcomes of severe adult pulmonary Streptococcus pyogenes infections that coincided with a high community caseload in central Scotland, UK. The pulmonary infections had high illness and death rates and were associated with socioeconomic deprivation, influenza A co-infection, and the M1UK lineage of S. pyogenes.
The association between respiratory viruses and secondary invasive pulmonary bacterial disease is recognized, but the proportion of pulmonary invasive group A Streptococcus (PiGAS) infections after seasonal influenza is low compared with those for other bacterial pathogens (e.g., Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus) (1,2). However, PiGAS has been shown to complicate epidemics of measles and, notably, the 1918–1919 influenza pandemic (3).
Winter 2022–23 saw a marked increase in influenza and associated group A Streptococcus (GAS) infections in the United Kingdom as well as globally (https://www.gov.uk/government/publications/group-a-streptococcal-infections-activity-during-the-2022-to-2023-season/group-a-streptococcal-infections-second-update-on-seasonal-activity-in-england-2022-to-2023). In autumn 2022, an unusually high number of pediatric GAS pleural empyema cases associated with human metapneumovirus co-infection was described in Scotland (4). After similar cases were observed in adults, we aimed to characterize the burden of PiGAS in adults and contrast it to published and local historical data.
We identified patients with pulmonary samples or blood cultures found positive for S. pyogenes by the National Health Service (NHS) of Greater Glasgow and Clyde (GGC), which serves a population of 1.4 million, during December 1, 2017–November 31, 2022, through the Laboratory Information Management System. We identified the same specimens from NHS Lothian (population 850,000) and GGC during December 1, 2022–February 28, 2023 (https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/mid-2021).
Samples assessed were sputum (inpatient), pleural fluid, endotracheal aspirate, bronchoalveolar lavage pulmonary tissue (postmortem), and blood cultures. We also identified S. pyogenes by molecular techniques (i.e., specific GAS PCR testing and 16s PCR). We defined cases as definite or probable PiGAS. A definite case required microbiologic criteria (e.g., S. pyogenes identified in blood or deep respiratory or pleural sample) and radiologic criteria (e.g., multifocal consolidation or pleural effusion or empyema or parenchymal necrosis) to be present. Probable cases were those with sputum samples in the microbiologic criteria and unifocal consolidation in the radiologic criteria, capturing patients meeting both criteria but not those of a definite case.
We extracted demographic, clinical, and laboratory data from electronic patient records. We derived Scottish Index of Multiple Deprivation (SIMD) scores by using postcodes. We also calculated Charlson comorbidity index scores. We referred S. pyogenes isolates to the Scottish Microbiology Reference Laboratory for M-typing and Illumina short read sequencing (5). We used an annotated whole genome–core genome multilocus sequence typing approach to compare isolate sequence data with a publicly available core genome multilocus sequence typing scheme implemented in Ridom SeqSphere+ version 8.5.1 (http://www.ridom.de/seqsphere), enabling assignment to the M1 lineages described in the European Nucleotide Archive (5,6). Currently, >200 recorded M-types are used to identify outbreaks and determine cluster management; M1 is most commonly associated with invasive disease (7).
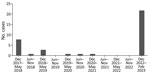
NHS GGC and Lothian provides public healthcare for ≈39% of Scotland’s population of 5.49 million (https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/mid-2021). Like other countries, the United Kingdom is undergoing a resurgence of S. pyogenes infections that began in September 2022 (https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON429). We identified 38 patients with PiGAS (30 definite, 8 probable) in the 3-month study period (22 in GGC, 16 in Lothian). In the previous 5-year period in GGC, we identified 15 cases (12 definite, 3 probable, 1 metastatic) (Figure 1).
We observed no significant difference in the median age between the 2022–23 cohort and historical records (45 [interquartile range (IQR) 26] years) vs. 57 [IQR 23.5] years). Both groups were healthy at baseline, having a median Charlson comorbidity index score of 0. We noted no significant difference in chronic respiratory underlying conditions. The 2022–23 cohort was associated with a more deprived SIMD postcode (median SIMD score of 3 vs. 5 for historical records). Other demographic, biochemical, and hematologic characteristics were comparable (Table). The PiGAS syndrome exhibits substantial leukopenia (median 0.53 [IQR 0.3–1] × 109 cells/L) with a normal median white cell count (9.5 [IQR 4–18.7] × 109 cells/L). Although respiratory symptoms predominated, diarrhea was reported in 18.4% (7/38) of cases in the 2022–23 outbreak. Microbiologically confirmed empyema was common, and a greater number of 2022–23 patients received an intercostal drain and exhibited radiologic evidence of empyema or pleural effusion (Table). Those characteristics, along with multifocal consolidation, were the radiologic hallmarks of PiGAS; cavitation also was common. A lower proportion of patients in the historical cohort had chest computed tomography results, precluding greater sensitivity (47% vs. 76%).
During 2017–2022, co-infecting respiratory viruses were varied, but in 2022–23, most patients tested positive for influenza A (Table; Figure 2). Only half of patients underwent an extended respiratory viral screen. Of typed S. pyogenes isolates from the current outbreak, 24/25 belonged to the M1UK lineage, contrasting with the historical cohort that involved a mixture of M types (M1, M12, M3.93, M44, and M5.23).
Europe is experiencing an increased incidence of invasive GAS disease (4). We report an unusually high incidence of severe PiGAS in adults from central Scotland. We also note an additional strong association with influenza A co-infection and the near-complete dominance of M1UK, contrasting with local and published precedent. M1 comprised 38% of adult and 58% of pediatric invasive GAS referrals in England during 2022–23, in contrast to the 96% we report (https://www.gov.uk/government/publications/group-a-streptococcal-infections-activity-during-the-2022-to-2023-season/group-a-streptococcal-infections-second-update-on-seasonal-activity-in-england-2022-to-2023). The clinical phenotype of severe, often rapidly fatal PiGAS disease in young healthy adults parallels outbreaks described around World War I and in institutional facilities (3,8). The M1UK lineage is emerging as a dominant lineage within M1 worldwide and often associated with invasive GAS (9–12).
The pathophysiology of PiGAS after a respiratory viral infection (influenza A in our cohort) is incompletely understood. In vitro and in vivo studies suggest prior influenza A infection increases both GAS adherence and internalization by binding to viral hyaluronic acid on the infected host cell surface, which is followed by increases in the abundance of, and access to, bacterial receptors and the GAS ligands fibrinogen and fibronectin (13). Influenza B is also implicated, both in the literature and locally during 2017–2018 (14).
M1 has an established association with severe disease (7). In particular, the M1UK strain appears to have an enhanced capability for transmission and virulence and is now the predominant strain in the United Kingdom (6). This strain exhibits a hypervirulent phenotype because of greater expression of streptococcal pyrogenic exotoxin A than global M1 strains. Case reports of severe rapidly fatal M1 PiGAS in young healthy patients echo outcomes seen in our cohort (15).
Modern molecular techniques have revolutionized our ability to investigate patterns of disease (e.g., widespread availability of rapid point-of-care tests for COVID-19 and influenza). We are experiencing a major outbreak of S. pyogenes infections with an unusual predilection for severe pulmonary disease in addition to the usual manifestations of disease by this pathogen, including distinctive viral and M-type associations in the winter and spring of 2022–23. The PiGAS phenotype we describe is similar to those from more sporadic reports identified from a review of published case series of severe pulmonary infections from S. pyogenes (Appendix). Historical outbreaks probably underreported coexistent viral infections because of a lack of accessible point-of-care tests. Similarly, only half of patients had an extended viral respiratory screen, and we therefore risk underreporting metapneumovirus cases, an agent notable locally in GAS empyema in children immediately before December 2022 (4). Although our cohort is small, it is comparatively large compared with the few described in the literature and notable for the short timeframe of cases captured.
Our study highlights a new aggressive pattern of S. pyogenes infections linked to the dominant circulating M1UK strain, manifesting as severe pulmonary disease and having a strong association with influenza A co-infection. Clinicians and public health officials need to be vigilant of such clinical manifestations while rates of iGAS remain high.
Dr. Davies is an infectious diseases and microbiology specialist trainee at the National Health Service Greater Glasgow and Clyde in Scotland. His primary research interests are GAS disease and microbiology diagnostic pathways.
Acknowledgment
We thank Pota Kalima for searching our Laboratory Information Management System to identify S. pyogenes specimens. We also thank Jörg Rothgänger for his assistance in preparing the core genome multilocus sequence typing scheme for use in SeqSphere+.
References
- Chertow DS, Memoli MJ. Bacterial coinfection in influenza: a grand rounds review. JAMA. 2013;309:275–82. DOIPubMedGoogle Scholar
- Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol. 2017;8:1041. DOIPubMedGoogle Scholar
- Morens DM, Taubenberger JK. A forgotten epidemic that changed medicine: measles in the US Army, 1917-18. Lancet Infect Dis. 2015;15:852–61. DOIPubMedGoogle Scholar
- Holdstock V, Twynam-Perkins J, Bradnock T, Dickson EM, Harvey-Wood K, Kalima P, et al. National case series of group A streptococcus pleural empyema in children: clinical and microbiological features. Lancet Infect Dis. 2023;23:154–6. DOIPubMedGoogle Scholar
- Friães A, Mamede R, Ferreira M, Melo-Cristino J, Ramirez M. Annotated whole-genome multilocus sequence typing schema for scalable high-resolution typing of Streptococcus pyogenes. J Clin Microbiol. 2022;60:
e0031522 . DOIPubMedGoogle Scholar - Zhi X, Li HK, Li H, Loboda Z, Charles S, Vieira A, et al. Emerging invasive group A Streptococcus M1UK lineage detected by allele-specific PCR, England, 2020. Emerg Infect Dis. 2023;29:1007–10. DOIPubMedGoogle Scholar
- Lindsay DSJ, Brown AW, Scott KJ, Denham B, Thom L, Rundell G, et al. Circulating emm types of Streptococcus pyogenes in Scotland: 2011-2015. J Med Microbiol. 2016;65:1229–31. DOIPubMedGoogle Scholar
- Crum NF, Russell KL, Kaplan EL, Wallace MR, Wu J, Ashtari P, et al. Pneumonia outbreak associated with group a Streptococcus species at a military training facility. Clin Infect Dis. 2005;40:511–8. DOIPubMedGoogle Scholar
- Rümke LW, de Gier B, Vestjens SMT, van der Ende A, van Sorge NM, Vlaminckx BJM, et al. Dominance of M1UK clade among Dutch M1 Streptococcus pyogenes. Lancet Infect Dis. 2020;20:539–40. DOIPubMedGoogle Scholar
- Davies MR, Keller N, Brouwer S, Jespersen MG, Cork AJ, Hayes AJ, et al. Detection of Streptococcus pyogenes M1UK in Australia and characterization of the mutation driving enhanced expression of superantigen SpeA. Nat Commun. 2023;14:1051. DOIPubMedGoogle Scholar
- Li Y, Nanduri SA, Van Beneden CA, Beall BW. M1UK lineage in invasive group A streptococcus isolates from the USA. Lancet Infect Dis. 2020;20:538–9. DOIPubMedGoogle Scholar
- Demczuk W, Martin I, Domingo FR, MacDonald D, Mulvey MR. Identification of Streptococcus pyogenes M1UK clone in Canada. Lancet Infect Dis. 2019;19:1284–5. DOIPubMedGoogle Scholar
- Herrera AL, Huber VC, Chaussee MS. The association between invasive group A streptococcal diseases and viral respiratory tract infections. Front Microbiol. 2016;7:342. DOIPubMedGoogle Scholar
- Aebi T, Weisser M, Bucher E, Hirsch HH, Marsch S, Siegemund M. Co-infection of Influenza B and Streptococci causing severe pneumonia and septic shock in healthy women. BMC Infect Dis. 2010;10:308. DOIPubMedGoogle Scholar
- Santagati M, Spanu T, Scillato M, Santangelo R, Cavallaro F, Arena V, et al. Rapidly fatal hemorrhagic pneumonia and group A Streptococcus serotype M1. Emerg Infect Dis. 2014;20:98–101. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleOriginal Publication Date: June 21, 2023
Table of Contents – Volume 29, Number 8—August 2023
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Peter Davies, Infectious Diseases Department, Queen Elizabeth University Hospital, 1345 Govan Rd, Glasgow, Scotland G51 4TF, UK
Top