Human Neural Larva Migrans Caused by Ophidascaris robertsi Ascarid
Mehrab E Hossain, Karina J. Kennedy, Heather L. Wilson, David Spratt, Anson Koehler, Robin B. Gasser, Jan Šlapeta, Carolyn A. Hawkins, Hari Priya Bandi, and Sanjaya N. Senanayake

Author affiliations: Canberra Health Services, Canberra, Australian Capital Territory, Australia (M. Hossain, K.J. Kennedy, H.L. Wilson, C.A. Hawkins, H. Bandi, S.N. Senanayake); Australian National University, Canberra (K.J. Kennedy, C.A. Hawkins, H. Bandi, S.N. Senanayake); Commonwealth Scientific and Industrial Research Organization Australian Capital Territory, Canberra (D. Spratt); University of Melbourne, Melbourne, Victoria, Australia (A. Koehler, R.B. Gasser); University of Sydney, Sydney, New South Wales, Australia (J. Šlapeta); The University of Sydney Institute for Infectious Diseases, Sydney (J. Šlapeta)
Main Article
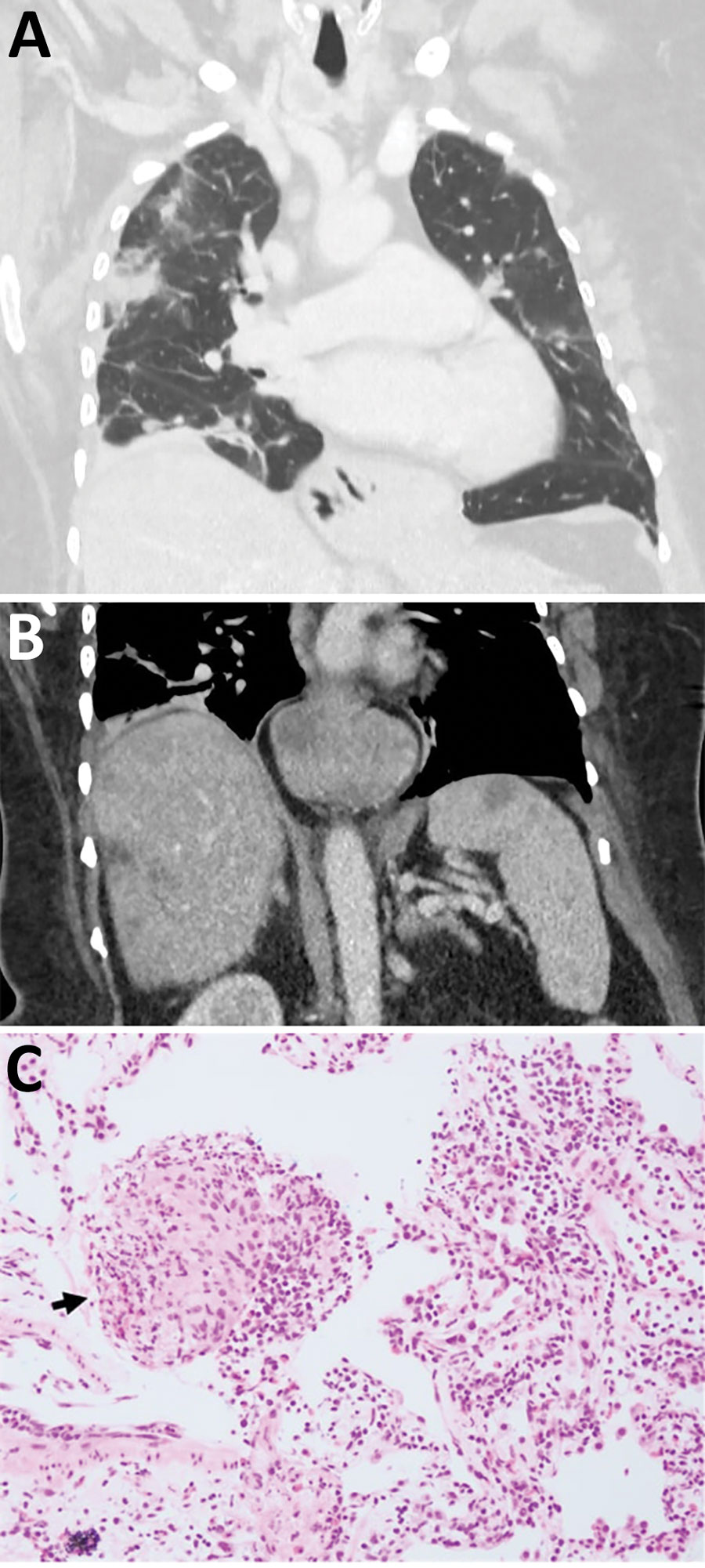
Figure 1
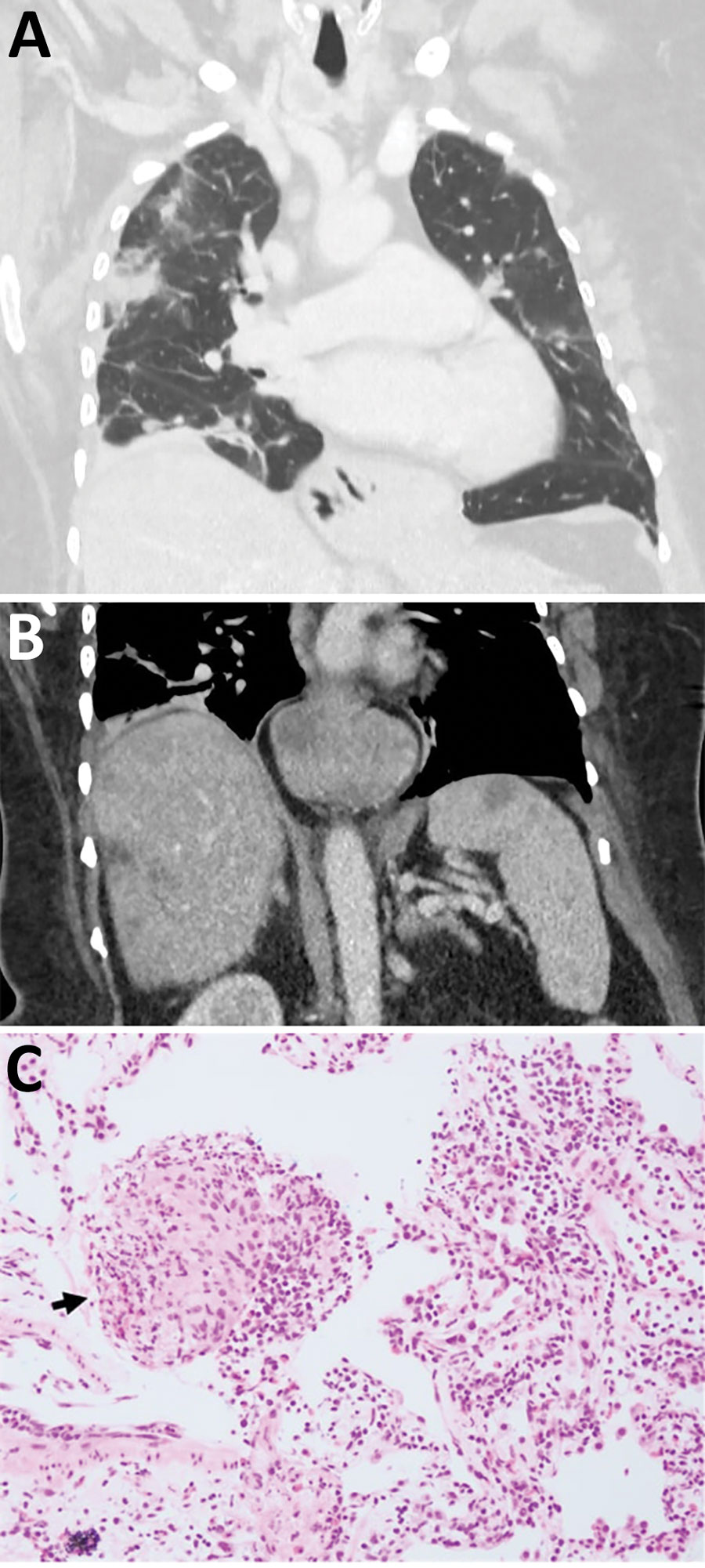
Figure 1. Early testing conducted during investigation of illness in a 64-year-old woman from southeastern New South Wales, Australia, who was later determined to have Ophidascaris robertsi nematode infection. A) Computed tomography scan of chest with venous contrast demonstrating multiple bilateral airspace opacities and nodules with a peripheral bronchovascular distribution. The opacities have surrounding ground-glass changes. Many were present in the patient’s study from a previous hospitalization; however, some had resolved while others were new, indicating a migratory pattern. B) Computed tomography scan of abdomen with venous contrast demonstrating multiple ill-defined hypoattenuated lesions within the liver and spleen. C) Hematoxylin and eosin stain (original magnification ×200) of a pulmonary lesion revealing prominent eosinophil infiltration of stroma and vessel walls. Arrow indicates a granuloma composed of histiocytes and eosinophils. The prominent eosinophilia was inconsistent with hypersensitivity pneumonitis, and the absence of vessel wall damage did not support a diagnosis of eosinophilic granulomatosis with polyangiitis.
Main Article
Page created: July 27, 2023
Page updated: August 20, 2023
Page reviewed: August 20, 2023
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions. Use of trade names is for identification only and does not imply endorsement by any of the groups named above.