Volume 29, Number 9—September 2023
Research Letter
Group A Streptococcus Meningitis in Adults, Denmark
Abstract
We report a 21-fold increase in group A Streptococcus meningitis in adults in Denmark during October 13, 2022–April 12, 2023, concurrent with an outbreak of invasive streptococcal disease. We describe clinical characteristics of the outbreak cases and prognosis for patients in comparison to those for previous sporadic cases.
Emergence of increased group A Streptococcus (GAS) disease, initially expressed as activity of scarlet fever in childhood, has been observed in multiple countries; some countries reported the toxigenic M1UK clone (1–3). A report from the Netherlands suggested an increase in GAS meningitis cases, mainly from the toxicogenic M1UK lineage (4). This increase is likely result of the rise in invasive GAS infections (5), because ≈1% of invasive GAS manifests as meningitis (6). However, it is unclear if this outbreak differs clinically from previous sporadic cases, as acknowledged by van der Putten et al. (4). To address this limitation, we compared all cases of GAS meningitis in adults in Denmark during 2015–2022 with cases during the outbreak, October 2022–April 2023.
The Danish Study Group for Infections of the Brain (DASGIB) has performed active, real-time nationwide surveillance of community-acquired bacterial meningitis in adults (>18 years of age) since January 1, 2015, as described previously (7). In brief, data on demographics, comorbidities, clinical signs and symptoms, microbiology and biochemical examinations, radiology, treatment, and outcome are aggregated in an online platform. The legal department of the North Denmark Region (record no. 2023-012693) and the Danish Board of Health (record nos. 3-3013-2579/1 and 3-3013-3168/1) approved the DASGIB database. Patient consent or permission from an ethical committee is not required.
For this study, a definition of GAS meningitis required (7) clinical symptoms suggestive of bacterial meningitis (e.g., headache, neck stiffness, fever, altered mental status) and either of the following criteria: positive culture or bacterial DNA/antigen analysis of cerebrospinal fluid (CSF); positive blood culture and CSF leukocytes >10 × 106 cells/L; or culture–confirmed otitis or mastoiditis and CSF leukocytes >10 × 106 cells/L. Incidence was computed as no. cases/no. adults in Denmark during each study period.
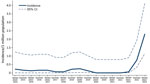
During January 1, 2015–October 12, 2022, we observed a total of 8 cases of GAS meningitis, corresponding to a mean of 0.11/1 million adults/6 months (Figure). Because of the increase in invasive GAS in Denmark beginning in October 2022 (8), we then assessed the incidence of GAS meningitis during October 13, 2022–April 12, 2023. We observed 11 cases of GAS meningitis in adults, corresponding to 2.32/1 million/6 months, an increase in incidence by a factor of 21. The diagnosis was confirmed by culture in 9 patients, whereas it was established by PCR in 2 patients for whom antimicrobial treatment began before lumbar puncture. We examined isolates of emm-1.0 type in 4 cases, emm-12.0 in 2 cases, and emm-87.0 in 1 case; isolate type was not available in 2 cases.
Patients with GAS meningitis had lower Glasgow Coma Scale scores at admission and higher CSF leukocyte counts in the last 6 months of the study than overall (Table); otherwise, clinical characteristics and prognosis did not differ between the 2 study periods. We observed a high percentage of patients with streptococcal infection in the upper respiratory tract (Table). We observed 2 serious complications, endophthalmitis (1 case) and subdural empyema (1 case), but no increase in deaths in the second study period.
We conclude that in October 2022–April 2023, an outbreak of GAS meningitis occurred in Denmark, showing a 21-fold increase in incidence compared with the baseline in previous years. The baseline incidence agrees with earlier findings in Denmark (9). Our case definition included cases confirmed by positive PCR of CSF, positive blood cultures or other cultures combined with CSF pleocytosis, and clinical manifestations of bacterial meningitis, in addition to positive CSF culture, which may explain why our incidence is higher than that recently reported for adults from the Netherlands (4).
The rise in invasive GAS infections was initially seen in children (5), but our study indicates an increase of severe infections in adults as well. The toxicogenic emm-1.0 type is currently the predominant strain in Denmark (8) and other countries (4,5). However, we found no differences in clinical characteristics or prognosis for GAS meningitis during this surge compared with those of previous years.
Dr. Nielsen is a clinical professor of infectious diseases at Aalborg University Hospital, Aalborg, Denmark. His research interest is infections in the brain, including bacterial meningitis.
References
- Lynskey NN, Jauneikaite E, Li HK, Zhi X, Turner CE, Mosavie M, et al. Emergence of dominant toxigenic M1T1 Streptococcus pyogenes clone during increased scarlet fever activity in England: a population-based molecular epidemiological study. Lancet Infect Dis. 2019;19:1209–18. DOIPubMedGoogle Scholar
- Demczuk W, Martin I, Domingo FR, MacDonald D, Mulvey MR. Identification of Streptococcus pyogenes M1UK clone in Canada. Lancet Infect Dis. 2019;19:1284–5. DOIPubMedGoogle Scholar
- Li Y, Nanduri SA, Van Beneden CA, Beall BW. M1UK lineage in invasive group A streptococcus isolates from the USA. Lancet Infect Dis. 2020;20:538–9. DOIPubMedGoogle Scholar
- van der Putten BCL, Vlaminckx BJM, de Gier B, Freudenburg-de Graaf W, van Sorge NM. Group A streptococcal meningitis with the M1UK variant in the Netherlands. JAMA. 2023;329:1791–2. DOIPubMedGoogle Scholar
- Guy R, Henderson KL, Coelho J, Hughes H, Mason EL, Gerver SM, et al. Increase in invasive group A streptococcal infection notifications, England, 2022. Euro Surveill. 2023;28:
2200942 . DOIPubMedGoogle Scholar - Davies HD, McGeer A, Schwartz B, Green K, Cann D, Simor AE, et al.; Ontario Group A Streptococcal Study Group. Invasive group A streptococcal infections in Ontario, Canada. N Engl J Med. 1996;335:547–54. DOIPubMedGoogle Scholar
- Bodilsen J, Larsen L, Brandt CT, Wiese L, Hansen BR, Andersen CØ, et al. Existing data sources for clinical epidemiology: the Danish Study Group of Infections of the Brain Database (DASGIB). Clin Epidemiol. 2021;13:921–33. DOIPubMedGoogle Scholar
- Statens Serum Institut. Increase in the number of group A streptococcal infections. 2023 [cited 2023 Jun 29]. https://www.ssi.dk/sygdomme-beredskab-og-forskning/sygdomsudbrud/streptokker
- Kjærgaard N, Bodilsen J, Justesen US, Schønheyder HC, Andersen CØ, Ellermann-Eriksen S, et al.; DASGIB Study Group. Community-acquired meningitis caused by beta-haemolytic streptococci in adults: a nationwide population-based cohort study. Eur J Clin Microbiol Infect Dis. 2019;38:2305–10. DOIPubMedGoogle Scholar
Figure
Table
Cite This ArticleOriginal Publication Date: July 21, 2023
Table of Contents – Volume 29, Number 9—September 2023
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Henrik Nielsen, Department of Infectious Diseases, Aalborg University Hospital, 18 Hobrovej, DK9000 Aalborg, Denmark
Top