Volume 2, Number 4—October 1996
Dispatch
Creutzfeldt-Jakob Disease in the United States, 1979-1994: Using National Mortality Data to Assess the Possible Occurrence of Variant Cases
Abstract
After a cluster of Creutzfeldt-Jakob disease (CJD) cases among unusually young patients was reported recently from the United Kingdom, we examined trends and the current incidence of CJD in the United States. We found that the age-adjusted CJD death rate in the United States is similar to published estimates of the crude incidence of CJD worldwide and has continued to be stable from 1979 through 1994. The number of CJD deaths in persons <45 years of age remained stable during this period. We found no evidence of the variant form of CJD.
Transmissible spongiform encephalopathies (TSE) are rare forms of progressive neurodegenerative disorders that affect both humans and animals (1). They are distinguished by long incubation periods, characteristic spongiform changes associated with neuronal loss, and a failure to induce inflammatory response (2). The prototype TSE in humans, Creutzfeldt-Jakob disease (CJD), occurs sporadically (approximately 90% of cases), through iatrogenic transmission of the infective agent (<1% of cases), or as an autosomal dominant inheritance (approximately 10% of cases) (3,4). CJD is a rapidly fatal dementing illness that occurs worldwide, with an estimated incidence of approximately one case per million persons. Unconventional agents termed prion proteins (PrPs), which are encoded by genes on chromosome 20, are considered the etiologic agent of CJD. The pathologic properties of these proteins lie in their three-dimensional configuration and their ability to recruit and influence normal PrPs to undergo similar conformational changes. The transmissibility of CJD has been verified with reports of iatrogenic transmission from a corneal transplant, electroencephalographic depth electrodes, neurosurgical procedures, cadaveric dura mater grafts, and pituitary hormone administration (5-11).
A cluster of CJD cases with a unique neuropathologic picture among unusually young patients in the United Kingdom (12), which was reported during a widespread epizootic of bovine spongiform encephalopathy (BSE), has alerted many countries, including the United States, to update their surveillance for CJD and look for similar cases (13). This increased attention, and the fact that CJD is rapidly and invariably fatal (14), prompted us to analyze the most current CJD deaths and update our analysis of national trends of CJD mortality in the United States. Because of concerns about the theoretical risk for transmission of CJD by blood transfusion, we also examined the mortality records for evidence of diseases associated with increased exposure to blood or blood products.
Multiple cause-of-death data for the United States from 1979 through 1994 were obtained from the National Center for Health Statistics, Centers for Disease Control and Prevention (CDC) (15), with 1994 data reported as provisional. Cause-of-death classifications were based on the Ninth Revision of the International Classification of Diseases (ICD-9) (16-18). CJD deaths were defined as those for which ICD-9 code 046.1 appeared as an entity-axis code. The alternative CJD ICD-9 code 331.5 is not valid in the United States (17,19,20). The case of a 3-year-old child with spongiform degeneration of infancy (ICD-9 code 046.1) was included in the study. We excluded the case of a 5-year-old child with Kawasaki disease (ICD-9 code 446.1) because CJD was not listed on the death certificate and the case of a 17-year-old patient who had had diffuse T-cell proliferative disease.
Annual CJD death rates were calculated as the number of CJD deaths per million persons, on the basis of U.S. resident population estimates, and standardized by the direct method, using the 1990 census population (21). Age-adjusted annual death rates were calculated by sex and race and for the United States overall; age-, sex-, and race-adjusted annual death rates were calculated by standard region (22). Risk ratios (RRs) with 95% confidence intervals (CIs) were calculated by Poisson regression analysis (23). Deaths were examined according to whether autopsy was indicated on the death certificate, as available from 1979 through 1993. We also examined other causes of death listed and searched the records for several diseases associated with increased exposure to blood or blood products, specifically hemophilia A (ICD-9 code 286.0), hemophilia B (ICD-9 code 286.1), thalassemia (ICD-9 code 282.4), and sickle cell disease (ICD-9 code 282.6).
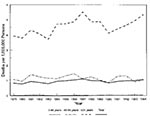
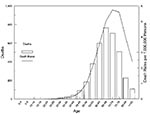
From 1979 through 1994, CJD was recorded as a cause of 3,642 deaths in the United States; 83.4% of these deaths had CJD recorded as the underlying cause. The average annual age-adjusted death rate during the study period was 0.95 deaths per million persons, from 0.78 in 1980 to 1.11 in 1987 (Figure 1). The mean age of death was 67 years (median age = 68 years). Approximately 98% of the deaths were among persons ≥45 years of age. The age-specific death rates were highest for persons in their 70s (Figure 2).
Although 52.9% of the deaths were in female patients, the age-adjusted death rate of male patients was slightly higher than that of female patients (RR = 1.16, 95% CI = 1.09-1.24; Table 1). In contrast to the death rate in age groups <60 years, the CJD death rate in age groups ≥60 years was higher in men than in women (Table 2). Most (95.2%) deaths were among whites. The age-adjusted death rate of whites was higher than that of blacks (RR = 2.66, 95% CI = 2.22-3.18) (Table 1). Other races accounted for only 1.4% of the CJD deaths, with an age-adjusted rate intermediate to that of blacks and whites. The death rate of blacks was lower than that of whites in each age group. Geographically, the age-sex-race-adjusted rate of the South was lower than that of each of the other regions. The previously noted differences by sex and race remained consistent for each region.
Approximately 80% of the CJD deaths were among persons ≥ 60 years of age. The average annual death rate during the study period of this age group was 4.58 per million persons (3.71 per million in 1983 to 5.52 per million persons in 1987) (Figure 1). Among persons 45 through 59 years of age, the average annual death rate was 1.15 per million persons (0.87 to 1.45 per million). Among persons <45 years of age, the annual death rate was consistently at or below 0.05 per million persons; the number of deaths among such young persons was zero in 1984 and eight in 1981 and 1993. Only five persons who died of CJD during the study period were younger than 30 years of age, and in any single year, there was no more than one such death. In the most recent 5-year period, 1990-1994, the only person with CJD in this young age group had received pituitary-derived human growth hormone.
None of the persons who died of CJD had hemophilia A, hemophilia B, thalassemia, or sickle cell disease mentioned on the death record. During 1979 through 1993, autopsies were performed on 907 persons who died of CJD-related causes (29.7% of those whose autopsy status was known). The proportion of autopsies ranged from 20.7% in 1993 to 37.8% in 1983. Autopsies of persons <45 years of age were indicated in 51.5% of the known deaths, while 30.2% and 29.0% were indicated in the 45- to 59-year-old and >= 60-year-old age groups, respectively.
During 1979 through 1994, the average annual age-adjusted death rate was 0.95 per million persons, which is consistent with published estimates of the crude incidence worldwide of one case per million persons (3,11). The addition of the 4 recent years of data to our previous report did not alter our initial findings (24). The previously reported racial differences in the U.S. CJD death rates were found again and should be further studied. In addition, no CJD-related deaths were found among persons with hemophilia A, hemophilia B, thalassemia, or sickle cell disease.
In 1994 and 1995, a cluster of 10 unusually young (median age at onset 28 years, range 16 to 39 years) CJD patients in the United Kingdom were reported with atypical clinical features (12). These features included behavioral change and dysesthesia when patients sought treatment, followed within weeks or months by a cerebellar syndrome, dementia, and myoclonus in the late stages, a duration of illness of at least 6 months, and electroencephalogram changes that were not diagnostic of CJD. These patients had a characteristic neuropathologic profile that consisted of severe spongiform change, neuronal loss, and astrocytosis in the basal ganglia and thalamus, with abundant kuru-type amyloid plaques surrounded by vacuoles in the cerebrum and cerebellum and PrP accumulation in high density shown by immunocytochemistry. These findings, coupled with the unusually young age of the patients, led to the conclusion that the clinicopathologic features constituted a new variant of CJD. A causal association with the BSE epizootic in British cattle was also hypothesized and recently supported by experimental evidence involving intracerebral inoculation of cynomolgus macaques with brain tissue obtained from cattle with BSE (25).
To help assess the purported uniqueness and distribution of the newly described CJD variant, CDC intensified CJD surveillance activities to seek evidence for the presence of this variant in the United States (13). In analyzing the U.S. multiple cause-of-death data, we did not find any increase in the number of CJD deaths among persons <45 years of age; also, there were no recent CJD deaths in persons <30 years of age, except for the death of the recipient of pituitary-derived human growth hormone (in contrast, five of the eight patients originally reported in the United Kingdom died before the age of 30). To supplement these findings in the United States, CDC also conducted active surveillance in its four Emerging Infections Program sites and in the Metropolitan Atlanta Active Surveillance Program in Georgia (total 1993 population 16.3 million) (13,26); 92% to 100% of neuropathologists and neurologists were contacted, and information was obtained on their patients who died of CJD from 1991 through 1995. Medical records and neuropathologic reports of decedents <55 years of age were also sought for review. Consistent with national mortality data, nine (10%) of the case patients were <55 years of age, only one case patient was <45 years of age, and no case patient was <30 years of age. Review of clinical and neuropathologic records of the nine patients <55 years of age did not show any with the variant form of CJD.
The validity of multiple cause-of-death data is potentially a problem because of possible coding and reporting discrepancies, including misdiagnoses (24). However, past reports have indicated that approximately 80% of histologically confirmed CJD patients were identified through death certificate searches, using national death registries (27). Furthermore, the consistency of data from the active surveillance sites with the national multiple cause-of-death data supports the conclusion that annual review of multiple cause-of-death data provides an efficient and cost-effective method to monitor CJD incidence (24,27). Active follow-up of reported CJD deaths in persons <55 years of age has been initiated in the United States to improve the national surveillance of potential cases of the newly described CJD variant. Access to more current national mortality data makes this data source even more beneficial in monitoring CJD deaths in the United States. Although currently available CJD surveillance data do not provide evidence for the variant CJD in the United States, ongoing CJD surveillance in this country and elsewhere, especially in the United Kingdom, will be critical for ultimately determining the geographic distribution of this illness and its possible relationship to BSE.
Acknowledgment
We thank Thomas J. Török, MD, for his support of the CJD surveillance efforts; Rima F. Khabbaz, MD, and Harry M. Rosenberg, PhD, for their critical review; Ken D. Kochanek, MA, Mary Ann Freedman, Deborah D. Ingram, PhD, and Charles E. Royer for technical assistance; Marilyn Velez, MPH, for manuscript preparation assistance; and John O'Connor, MS, for editorial assistance.
References
- DeArmond SJ, Prusiner SB. Etiology and pathogenesis of prion diseases. Am J Pathol. 1995;146:785–811.PubMedGoogle Scholar
- Budka H, Aguzzi A, Brown P, Brucher J, Bugiani O, Gullotta F, Neuropathalogical diagnostic criteria for Creutzfeldt-Jakob disease and other human spongiform encephalopathies [Prion diseases]. Brain Pathol. 1995;5:459–66. DOIPubMedGoogle Scholar
- Masters CL, Harris JO, Gajdusek DC, Gibbs CJJ, Bernoulli C, Asher DM. Creutzfeldt-Jakob disease: patterns of worldwide occurrence and the significance of familial and sporadic clustering. Ann Neurol. 1979;5:177–88. DOIPubMedGoogle Scholar
- Will RG. Epidemiology of Creutzfeldt-Jakob disease. Br Med Bull. 1993;49:960–70.PubMedGoogle Scholar
- Gibbs Jr CJ, Gajdusek DC, Asher DM, Alpers MP, Beck E, Daniel PM, . Creutzfeldt-Jakob disease (spongiform encephalopathy): transmission to the chimpanzee. Science. 1968;161:388–9. DOIPubMedGoogle Scholar
- Duffy P, Wolf J, Collins G, DeVoe AG, Streeten B, Cowen D. Possible person-to-person transmission of Creutzfeldt-Jakob disease. N Engl J Med. 1974;290:692–3.PubMedGoogle Scholar
- Bernoulli C, Siegfried J, Baumgartner G, Regli F, Rabinowicz T, Gajdusek DC, . Danger of accidental person-to-person transmission of Creutzfeldt-Jakob disease by surgery. Lancet. 1977;1:478–9.PubMedGoogle Scholar
- Will RG, Matthews WB. Evidence for case-to-case transmission of Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 1982;45:235–8. DOIPubMedGoogle Scholar
- Centers for Disease Control. Rapidly progressive dementia in a patient who received a cadaveric dura mater graft. MMWR. 1987;36:49–50, 55.PubMedGoogle Scholar
- Fradkin JE, Schonberger LB, Mills JL, Gunn WJ, Piper JM, Wysowski DK, Creutzfeldt-Jakob disease in pituitary growth hormone recipients in the United States. JAMA. 1991;265:880–4. DOIPubMedGoogle Scholar
- Brown P, Preece MA, Will RG. "Friendly fire" in medicine: hormones, homografts, and Creutzfeldt-Jakob disease. Lancet. 1992;340:24–7. DOIPubMedGoogle Scholar
- Will RG, Ironside JW, Zeidler M, Cousens SN, Estibeiro K, Alperovitch A, A new variant of Creutzfeldt-Jakob disease in the UK. Lancet. 1996;347:921–5. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. World Health Organization consultation on public health issues related to bovine spongiform encephalopathy and the emergence of a new variant of Creutzfeldt-Jakob disease. MMWR. 1996;45:295–6, 303.PubMedGoogle Scholar
- Brown P, Cathala F. Creutzfeldt-Jacob disease in France. In: Hadlow WJ, Prusiner SB, eds. Slow transmissible diseases of the nervous system. New York: Academic Press, 1979;vol 1: 213-27.
- U.S. Department of Health and Human Services. Vital statistics mortality data, multiple cause detail, 1979-1993. Public use data tape contents and documentation package. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics, 1996.
- U.S. Department of Health and Human Services. Vital statistics of the United States, 1988, vol II, mortality, Part A. Washington, D.C.: Public Health Service, Centers for Disease Control, National Center for Health Statistics; DHHS pub. no. (PHS) 91-1101; 1991.
- World Health Organization. Manual of the international statistical classification of diseases, injuries, and causes of death. Based on recommendations of the 9th revision conference, 1975, and adopted by the 29th World Health Assembly. Geneva: World Health Organization, 1977.
- Israel RA, Rosenberg HM, Curtin LR. Analytical potential for multiple cause-of-death data. Am J Epidemiol. 1986;124:161–79.PubMedGoogle Scholar
- National Center for Health Statistics. Instruction manual, part 9. ICD-9 underlying cause of death lists for tabulating mortality statistics. Hyattsville, MD: Public Health Service, 1979.
- National Center for Health Statistics. Instruction manual: part 11. Computer edits for mortality data. Hyattsville, MD: Public Health Service, 1989.
- Bureau of Census. Intercensal estimates of the population by age, sex, and race: 1970-1993. Washington, DC: Bureau of Census, 1996.
- Armitage P, Berry G. Statistical methods in medical research. Oxford: Blackwell Scientific Publications, 1987.
- Kleinbaum DG, Kupper LL, Muller KE, eds. Applied regression analysis and other multivariable methods. Boston: PWS-KENT Publishing Company, 1988.
- Holman RC, Khan AS, Kent J, Strine TW, Schonberger LB. Epidemiology of Creutzfeldt-Jakob disease in the United States, 1979-1990: Analysis of national mortality data. Neuroepidemiology. 1995;14:174–81. DOIPubMedGoogle Scholar
- Lasmezas CI, Deslys JP, Demaimay R, Adjou KT, Lamoury F, Dormont D. BSE transmission to macaques. Nature. 1996;381:743–4. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Surveillance for Creutzfeldt-Jakob Disease--United States. MMWR. 1996;45:665–8.PubMedGoogle Scholar
- Davanipour Z, Smoak C, Bohr T, Sobel E, Liwnicz B, Chang S. Death certificates: an efficient source for ascertainment of Creutzfeldt-Jakob disease cases. Neuroepidemiology. 1995;14:1–6. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 2, Number 4—October 1996
| EID Search Options |
|---|
|
|
|
|
|
|