Volume 29, Number 8—August 2023
Dispatch
Pediatric SARS-CoV-2 Seroprevalence, Oregon, USA, November 1, 2020–June 30, 2022
Abstract
We estimated SARS-CoV-2 seroprevalence in children in Oregon, USA, at 6 time points. Seroprevalence increased linearly during November 2020–December 2021 and peaked in February 2022 at 38.8% (95% CI 32.8%–46.5%). We observed no increase in the seroprevalence trend after widespread school reopening. Seroprevalence estimates complement case-based cumulative incidence.
Through June 30, 2022, a total of 140,820 pediatric cases of COVID-19 had been reported in Oregon, USA, representing ≈17.3% of all reported COVID-19 cases in the state. However, understanding the true burden of pediatric COVID-19 infection poses a challenge. Children are more likely to have asymptomatic or mild disease, and pediatric infections are, therefore, less likely to be reported to public health authorities (1,2). Clarifying pediatric SARS-CoV-2 prevalence is important because it is well established that children can transmit SARS-CoV-2 to other children and adults (3,4). In addition, children are at risk for severe complications, including postinfectious multisystem inflammatory syndrome in children (MIS-C) (5). Seroprevalence provides additional insight into the true cumulative incidence of COVID-19 in children.
To estimate the seroprevalence of COVID-19 infection in children in Oregon, blood was collected in 6 phases during November 1, 2020–June 30, 2022, from a cross-sectional convenience sample and tested for SARS-CoV-2 nucleocapsid IgG, in alignment with the World Health Organization seroepidemiologic investigation protocol (6). We recruited Oregon healthcare facilities with >6 inpatient pediatric hospital beds to participate in this study and asked them to provide <100 specimens per phase; 5 facilities agreed to participate. We asked facilities to submit random samples of deidentified residual serum samples from patients <17 years of age visiting any ambulatory, emergency, or inpatient healthcare setting and to include specimen collection date and patient’s date of birth. The initial round of sampling was November 1–December 31, 2020. We extended the project timeline and collected additional samples bimonthly during October 1, 2021–June 30, 2022.
Specimens were stored according to instructions provided by the test manufacturer and transported to the Oregon State Public Health Laboratory (Hillsboro, Oregon, USA). We tested the specimens with a SARS-CoV-2 IgG assay (Abbott Laboratories, https://www.abbott.com), which detects antibodies to the nucleocapsid protein of SARS-CoV-2. Nucleocapsid IgG immunoassays detect antibodies produced after infection and do not detect antibodies produced after vaccination with vaccines licensed for use in the United States. The manufacturer reports test sensitivity (Sn) of 100% (95% CI 95.9%–100%) at >14 days past symptom onset and specificity (Sp) of 99.6% (95% CI 99.1%–99.9%). We calculated unadjusted seroprevalence estimates for each collection period as the percentage of all specimens that tested positive. We adjusted seroprevalence estimates for test performance as observed prevalence + (specificity – 1) divided by sensitivity + (specificity – 1) (7).
We obtained adjusted 95% CI with parametric bootstrapping (8). Because SARS-CoV-2 antibody detection is dependent on test timing and assay, we also performed sensitivity analysis with seroprevalence estimates adjusted for declining assay sensitivity over 130 days of convalescence (9,10) (Appendix) We used R version 4.1.2 (The R Foundation for Statistical Computing, https://www.r-project.org) for all analyses.
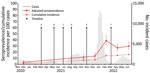
We collected 1,869 specimens from 5 facilities during 6 phases. The mean number of specimens collected during each phase was 312 (range 215–438). Overall, we observed a strong linear trend (p = 0.001) for adjusted seroprevalence estimates during November 1, 2020—December 31, 2021; seroprevalence increased by ≈0.7% per 4-week period during that period (Figure). After the Omicron surge, adjusted seroprevalence increased sharply from 13.4% (95% CI 9.8%–18.4%) in December 2021 to 38.8% (95% CI 32.8%–46.5%) in February 2022. Adjusted seroprevalence estimates then decreased but did not return to pre–February 2022 levels (Table). Adjusting for declining assay sensitivity over time led to estimates that were larger and less stable over convalescence (Appendix).
Our repeated cross-sectional study estimated pediatric seroprevalence in Oregon at 6 points across 20 months of pandemic response. During that period, K–12 public schools reopened statewide, vaccines were rolled out in 2 phases to children 12–15 and 5–11 years of age, and universal indoor masking mandates remained in place during the school year until March 12, 2022 (Figure). After widespread school reopening in early 2021, with a masking mandate in place, pediatric seroprevalence in October 2021 was 11.8%, and no increase in trend was observed. The only sudden increase in pediatric seroprevalence followed the Omicron surge in early 2022. Seroprevalence began to decline after its February 2022 peak but did not return to pre-Omicron levels.
Seroprevalence can provide more accurate estimates of the true cumulative incidence of SARS-CoV-2 infection than case reporting to public health entities does, because seroprevalence data capture evidence of previous infection in persons who are not tested through the traditional healthcare system because of asymptomatic or mild disease, lack of testing access, refusal to test, or self-testing at home (11). We estimated 1.7–2.8 times the number of infections in children from seroprevalence than the reported cumulative incidence in Oregon (Figure). This total is a lower degree of underascertainment than had been reported in seroprevalence studies of children during May–July 2021 in the United States (1).
Because seroprevalence studies measure circulating antibodies at the time of testing and SARS-CoV-2 antibodies wane over time, seroprevalence is limited in its ability to estimate cumulative incidence as the pandemic progresses (12). In addition, time to seroreversion is dependent on the target antigen and the assay used (9,10,13). One study found a mean time of seroreversion of 19 weeks with use of the Abbott IgG immunoassay, compared with 91 weeks using the Roche pan-Ig immunoassay (13). In our study, waning immunity was apparent as estimated seroprevalence decreased following its Omicron-related peak in February 2022. A sensitivity analysis, adjusting for declining sensitivity of the Abbott immunoassay, partially accounted for this decline; more complex models have been published to correct seroprevalence estimates for assay performance (13). However, now that essentially all persons in the United States have been infected with SARS-CoV-2, the use of an assay with waning sensitivity to remote infections may permit continued examination of more granular temporal changes in seroprevalence in the context of changing policy and variant predominance.
The Centers for Disease Control and Prevention began collecting pediatric seroprevalence data for the Multistate Assessment of SARS-CoV-2 Seroprevalence in Commercial Labs (MASS-C) in July 2020 (14). MASS-C estimates of pediatric seroprevalence in Oregon are consistently higher than our estimates (15). Although MASS-C similarly derives its estimates from a convenience sample of serum specimens, testing is performed with the Roche antinucleocapsid total antibody assay (14). In addition, MASS-C estimates are weighted for age and sex, and the demographics of that pediatric population may demographically differ from our study population.
We obtained our convenience sample from children who received care from large pediatric healthcare facilities throughout the state; findings are not necessarily generalizable to the entire state pediatric population. Limitations of seroprevalence testing include lack of antibody development by some infected persons (including immunocompromised persons) and, in others, waning of antibodies to undetectable levels, such that seroprevalence becomes a less reliable proxy for cumulative incidence as the duration of the pandemic increases (12).
Traditional public health case-based reporting substantially underestimates the burden of COVID-19. In this study, seroprevalence estimates made using an assay with waning sensitivity to remote infections provided evidence that the widespread reopening of schools with a masking mandate in place did not increase the rate of pediatric SARS-CoV-2 infections. Case-based cumulative incidence estimates failed to capture the magnitude of the Omicron variant’s effect on Oregon’s pediatric population. Serosurveillance of SARS-CoV-2 antibodies in Oregon’s pediatric population complements case-based surveillance and can inform future public health interventions and policy decisions.
Dr. Falender is a Council of State and Territorial Epidemiologists applied epidemiology fellow at Oregon Health Authority, working in acute and communicable disease prevention. Her research interests include emerging infectious diseases and One Health.
Acknowledgment
This study and report were supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by the Centers for Disease Control and Prevention (cooperative agreement no. 1NU38OT000297-03-00).
References
- O’Brien SC, Cole LD, Albanese BA, Mahon A, Knight V, Williams N, et al. SARS-CoV-2 seroprevalence compared with confirmed COVID-19 cases among children, Colorado, USA, May–July 2021. Emerg Infect Dis. 2023;29:929–36. DOIPubMedGoogle Scholar
- Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088–95. DOIPubMedGoogle Scholar
- Laxminarayan R, Wahl B, Dudala SR, Gopal K, Mohan B C, Neelima S, et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science. 2020;370:691–7. DOIPubMedGoogle Scholar
- Szablewski CM, Chang KT, Brown MM, Chu VT, Yousaf AR, Anyalechi N, et al. SARS-CoV-2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1023–5. DOIPubMedGoogle Scholar
- Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al.; California MIS-C Response Team. COVID-19–associated multisystem inflammatory syndrome in children—United States, March–July 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1074–80. DOIPubMedGoogle Scholar
- World Health Organization. Population-based age-stratified seroepidemiological investigation protocol for COVID-19 virus infection, 17 March 2020. Geneva: The Organization; 2020.
- Reiczigel J, Földi J, Ozsvári L. Exact confidence limits for prevalence of a disease with an imperfect diagnostic test. Epidemiol Infect. 2010;138:1674–8. DOIPubMedGoogle Scholar
- Henrion MY. bootComb—an R package to derive confidence intervals for combinations of independent parameter estimates. Oxford: Oxford University Press; 2021.
- Peluso MJ, Takahashi S, Hakim J, Kelly JD, Torres L, Iyer NS, et al. SARS-CoV-2 antibody magnitude and detectability are driven by disease severity, timing, and assay. Sci Adv. 2021;7:
eabh3409 . DOIPubMedGoogle Scholar - Stone M, Grebe E, Sulaeman H, Di Germanio C, Dave H, Kelly K, et al. Evaluation of commercially available high-throughput SARS-CoV-2 serologic assays for serosurveillance and related applications. Emerg Infect Dis. 2022;28:672–83. DOIPubMedGoogle Scholar
- Sutton M, Cieslak P, Linder M. Notes from the field: seroprevalence estimates of SARS-CoV-2 infection in convenience sample—Oregon, May 11–June 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1100–1. DOIPubMedGoogle Scholar
- Post N, Eddy D, Huntley C, van Schalkwyk MCI, Shrotri M, Leeman D, et al. Antibody response to SARS-CoV-2 infection in humans: A systematic review. PLoS One. 2020;15:
e0244126 . DOIPubMedGoogle Scholar - García-Carreras B, Hitchings MDT, Johansson MA, Biggerstaff M, Slayton RB, Healy JM, et al. Accounting for assay performance when estimating the temporal dynamics in SARS-CoV-2 seroprevalence in the U.S. Nat Commun. 2023;14:2235. DOIPubMedGoogle Scholar
- Bajema KL, Wiegand RE, Cuffe K, Patel SV, Iachan R, Lim T, et al. Estimated SARS-CoV-2 Seroprevalence in the US as of September 2020. JAMA Intern Med. 2021;181:450–60. DOIPubMedGoogle Scholar
- US Centers for Disease Control and Prevention. COVID data tracker: national commercial lab pediatric antibody seroprevalence. February 2, 2023 [cited 2023 Feb 6]. https://covid.cdc.gov/covid-data-tracker/#pediatric-seroprevalence
Figure
Table
Cite This ArticleOriginal Publication Date: July 12, 2023
Table of Contents – Volume 29, Number 8—August 2023
| EID Search Options |
|---|
|
|
|
|
|
|
Please use the form below to submit correspondence to the authors or contact them at the following address:
Melissa Sutton, Public Health Division, Oregon Health Authority, 800 NE Oregon St, Ste 772, Portland OR 97232, USA
Top