Volume 28, Number 9—September 2022
Research
Rapid Adaptation of Established High-Throughput Molecular Testing Infrastructure for Monkeypox Virus Detection
Abstract
Beginning in May 2022, a rising number of monkeypox cases were reported in non–monkeypox-endemic countries in the Northern Hemisphere. We adapted 2 published quantitative PCRs for use as a dual-target monkeypox virus test on widely used automated high-throughput PCR systems. We determined analytic performance by serial dilutions of monkeypox virus reference material, which we quantified by digital PCR. We found the lower limit of detection for the combined assays was 4.795 (95% CI 3.6–8.6) copies/mL. We compared clinical performance against a commercial manual orthopoxvirus research use only PCR kit by using clinical remnant swab samples. Our assay showed 100% positive (n = 11) and 100% negative (n = 56) agreement. Timely and scalable PCR tests are crucial for limiting further spread of monkeypox. The assay we provide streamlines high-throughput molecular testing for monkeypox virus on existing broadly established platforms used for SARS-CoV-2 diagnostic testing.
In May 2022, an unusually high number of monkeypox cases were reported in countries in western Europe and North America; by May 29, 2022, 257 laboratory-confirmed infections were reported from Spain, Portugal, the United Kingdom, Canada, and the United States, sparking fear of another global outbreak on the heels of the continuing SARS-CoV-2 pandemic (1–4). Endemic transmission of the monkeypox virus (MPXV), a species of the Orthopoxvirus genus, is thought to be limited to central and western Africa, where both zoonotic (≈22%–72% of cases) and person-to-person transmission contribute to disease burden (5). Previous clusters outside Africa have usually been traceable to animal sources rather than to human-to-human transmission (6). In contrast, the 2022 cases seem to have occurred without any links to animal sources and have been concentrated in, but not exclusive to, men who have sex with men (7). The sudden appearance of infections in several non–monkeypox-endemic countries suggested that undetected transmission might have taken place for some time but that recent events could have served as a catalyst for spread (1).
The ongoing SARS-CoV-2 pandemic has demonstrated the potential and value of highly automated high-throughput molecular testing in outbreak scenarios. We aimed to rapidly adapt existing automated molecular testing infrastructure for SARS-CoV-2 in a large tertiary-care hospital in Hamburg, Germany, for detection of MPXV from clinical samples, thereby creating the capacity for high-throughput testing and quick turnaround times, if needed.
Multiplex Assay Setup
On the basis of diagnostic testing during the SARS-CoV-2 pandemic (8; C. Manohar et al., unpub. data, https://doi.org/10.1101/2021.10.13.21264919), we chose a dual-target approach, in which 1 assay targets a conserved sequence of the Orthopoxvirus genus, not including variola major or minor viruses (9), and the other targets a MPXV-specific sequence (10) (Table 1). The cobas 5800, 6800, and 8800 systems (Roche Diagnostics, https://diagnostics.roche.com) use a spike-in RNA full process control that is added automatically during extraction. The corresponding internal control assay is preloaded in the open channel reagent for use with cobas omni Utility Channel (Roche Diagnostics) (Table 2). We modified and optimized all assays for use on cobas 5800, 6800, and 8800 systems, including 2′O-methyl-RNA-modified primers and internal quenchers for TaqMan probes, as previously described (11).
In Silico Evaluation
As part of a support request for Utility Channel applications, we submitted all sequences of the duplex assay to Roche Diagnostics for evaluation of inclusivity and potential primer-probe interactions. The submitted sequences were aligned to currently available MPXV and orthopoxvirus sequences available in public databases.
Analytical Performance Evaluation
We conducted technical performance evaluations for the assays according to new European Union regulations (Regulation 2017/746 EU IVDR, https://euivdr.com). For reference material, we used inactivated cell culture supernatant containing MPXV recovered from a clinical case in central Africa in 1987 (12) and inactivated modified vaccinia virus Ankara (MVA) SARS-CoV-2 vaccine. To obtain a quantitative MPXV standard, we purified nucleic acids by using a MagNA-pure96 extractor and Viral NA Small Volume Kit (Roche Diagnostics) and analyzed on a QIAcuity digital PCR instrument (QIAGEN, https://www.qiagen.com) in conjunction with 3 different previously described quantitative PCRs (qPCRs): 1 for nonvariola (NVAR) orthopoxviruses (9); 1 for MPXV (10); and the research-use only (RUO) LightMix Modular Orthopoxvirus Assay (TIB MOLBIOL, https://www.tib-molbiol.de).
We determined the lower limit of detection by serial 2-fold dilution of MPXV standard in universal transport medium from 100 to 0.78 copies/mL and 21 repeats per dilution step. Using MedCalc statistical software (https://www.medcalc.org), we determined the limit for 95% probability of detection. We assessed linearity by 10-fold serial dilution of MPXV standard (5 repeats per dilution step) at concentrations of ≈101–107 copies/mL. We determined linearity and intra-assay variability by using Validation Manager software (Finbiosoft, https://finbiosoft.com). Concentrations represent copies per mL of specimen. For empirical inclusivity and exclusivity testing, we used the assay to test a set of 53 samples, including clinical samples, reference material, and external quality controls from a range of bloodborne and respiratory pathogens (Appendix Table 1). We used an experimental MVA vector-based SARS-CoV-2 vaccine as reference material for a non-MPXV orthopoxvirus.
Clinical Evaluation and Follow-Up Samples
For clinical validation, we used the RUO LightMix Modular Orthopoxvirus assay as reference test, which we performed according to manufacturer’s recommendation by using the MagNA-pure96 system with 200-µL extraction volume. In total, we tested 67 clinical samples consisting of respiratory, skin, and genital swab samples with both assays. Of those samples, 11 were positive for MPXV DNA, which we obtained from 2 confirmed clinical cases in Hamburg, Germany. We analyzed 33 consecutive clinical samples from the same 2 patients and 2 additional cases by using the duplex assay (Appendix Table 2). The clinic provided globalized patient characteristics.
In Silico Analysis
We did not detect any concerning oligo interactions (Appendix Figure 1). Target-1: NVAR was still a 100% match for all but 1 MPXV sequence, which had 1 low-risk mismatch. NVAR also had high sequence similarity with many other orthopoxviruses but might not be optimal for reliable detection of camelpox or cowpox (Appendix Figure 2). Target-2: MPOX is a perfect match for almost all Congo Basin strain MPXV sequences but has a known mismatch for West Africa strain sequences in the probe region. This mismatch is expected to slightly reduce relative fluorescence increase signals, as demonstrated in the clinical sample set. Other orthopoxviruses have extensive sequence mismatches with this assay and are not expected to produce detectable signals (Appendix Figure 3).
Analytical performance
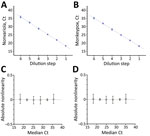
We determined LoD was 9.697 (95% CI 7.424–15.327) copies/mL for the NVAR assay and 6.359 (95% CI 4.908–10.110) copies/mL for the MPOX assay by probability of detection analysis. Overall LoD for both targets combined was 4.795 (95% CI 3.598–8.633) copies/mL. We compiled hit rates (Table 3) and probability of detection plots (Appendix Figure 4) for the assay. The assay showed excellent linearity. Cycle threshold (Ct) values were 37–18, ≈101–107 copies/mL, and pooled SD and 95% CI were within linear range: Ct 0.194, SD 0.0662% for NVAR; Ct 0.175, SD 0.618% for MPXV (Figure 1).
No false positives occurred within the inclusivity-exclusivity set. The MVA vector vaccine was correctly detected by the NVAR assay, and not by the MPXV assay (Appendix Table 1).
Clinical Evaluation
In total, we tested 67 clinical samples, consisting of respiratory, skin, and genital swab samples, with both assays. Of those, 11 samples obtained from 2 confirmed clinical monkeypox case-patients in Hamburg, Germany, were positive for MPXV DNA. We noted 100% positive (11/11) and 100% negative agreement (56/56) for the 2 assays (Figure 2).
Results from Different Sample Types and Timepoints
Another 33 clinical samples were longitudinally collected from 4 patients, all of whom were male, 20–40 years of age, and had 6–50 skin lesions; 1 patient had known HIV infection under treatment. Lesion swabs generated Ct values of 13.3–16.1, oropharyngeal swabs Ct values of 13.1–33.3, and blood samples Ct values of 30.3–38.4. A small sample set of urine had only low concentrations of viral DNA, Ct 31.1–37.8. A single patient provided seminal fluid, which had Ct values of 32.9 for the NVAR assay and 33.9 for the MPXV assay when diluted in guanidine hydrochloride solution (Appendix Table 2).
The trajectory of the ongoing MPXV outbreak in Europe and North America has many uncertainties. However, the World Health Organization acknowledges that known clusters represent a change in transmission pattern and emphasizes the need to limit further spread (1). Broad availability of molecular testing with short turnaround times is a crucial prerequisite for reducing monkeypox spread.
We adapted 2 established nonvariola orthopoxvirus and MPXV qPCR assays (9,10) as a duplex test for the cobas 5800, 6800, and 8800 fully automated sample-to-result platforms, which are widely used for high-throughput SARS-CoV-2 diagnostic testing (13). Both assays have been validated extensively against other orthopoxvirus species in previous studies (9,10) and remain inclusive and highly specific for in silico analysis with currently available monkeypox sequences. We demonstrated excellent analytical performance of the duplex assay, showing single-digit detection limits and near-perfect PCR efficiency. A spike-in full-process control assay, similar to commercial in vitro diagnostic assays, already is included in the open channel reagents we used.
Our institution confirmed 4 clinical cases of monkeypox, and we used the initial clinical samples as our clinical positive set. Although the assay was only validated on swab samples, we also detected MPXV DNA in EDTA plasma, urine, and seminal fluid diluted in guanidine hydrochloride solution without any method adaptations. Among all tested clinical samples positive for MPXV DNA, swabs of skin lesions consistently yielded early Ct values in the low- to mid-teens, indicating exceedingly high viral DNA loads, which might be a concern for both personnel safety and contamination risks. Viral DNA was readily detectable in oropharyngeal swab samples, as previously reported (2,14). Likewise, EDTA plasma samples were consistently positive but had later Ct values, mostly around 30. Further studies could evaluate the practical usefulness of plasma or urine for monkeypox diagnostic purposes or longitudinal viral load monitoring. Our data regarding MPXV DNA in different clinical specimen types are well in line with other published studies (2,14); overall, skin lesion swab samples appeared to be best suited for diagnostic purposes based on our sample set.
In conclusion, we provided technical performance evaluation for a laboratory-developed duplex qPCR assay for MPXV detection for use on the cobas 5800, 6800, and 8800 high-throughput systems. The assay we describe enables laboratories to adapt existing automated SARS-CoV-2 molecular testing infrastructure for a potential large-scale monkeypox outbreak.
Dr. Nörz is a fellow in the institute of Medical Microbiology, Virology and Hygiene at University Medical Center Hamburg-Eppendorf, Hamburg, Germany. His research interests include molecular diagnostics for infectious diseases and quantitative PCR assay design.
Acknowledgments
M.L. and D.N. received speaker honoraria and related travel expenses from Roche Diagnostics.
M.L., S.P., and D.N. conceptualized and supervised the study. H.T.T., D.N., and P.E. performed the experiments. K.G. performed data analysis. D.N., M.L., S.P., N.F., S.S., M.M.A. and M.A. wrote and edited the manuscript. All authors agreed to the publication of the final manuscript.
References
- World Health Organization. Disease outbreak news: multi-country monkeypox outbreak in non-endemic countries 29 May 2022 [cited 2022 Jun 7]. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON388
- Antinori A, Mazzotta V, Vita S, Carletti F, Tacconi D, Lapini LE, et al.; INMI Monkeypox Group. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro Surveill. 2022;27:
2200421 . DOIPubMedGoogle Scholar - Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, et al.; UKHSA Monkeypox Incident Management team; Monkeypox Incident Management Team. Community transmission of monkeypox in the United Kingdom, April to May 2022. Euro Surveill. 2022;27:
2200422 . DOIPubMedGoogle Scholar - Perez Duque M, Ribeiro S, Martins JV, Casaca P, Leite PP, Tavares M, et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 2022;27:
2200424 . DOIPubMedGoogle Scholar - Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, Baer LR, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16:
e0010141 . DOIPubMedGoogle Scholar - Reed KD, Melski JW, Graham MB, Regnery RL, Sotir MJ, Wegner MV, et al. The detection of monkeypox in humans in the Western Hemisphere. N Engl J Med. 2004;350:342–50. DOIPubMedGoogle Scholar
- Adalja A, Inglesby T. A novel international monkeypox outbreak. Ann Intern Med. 2022 May 24 [Epub ahead of print].
- Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:25. DOIPubMedGoogle Scholar
- Li Y, Olson VA, Laue T, Laker MT, Damon IK. Detection of monkeypox virus with real-time PCR assays. J Clin Virol. 2006;36:194–203. DOIPubMedGoogle Scholar
- Shchelkunov SN, Shcherbakov DN, Maksyutov RA, Gavrilova EV. Species-specific identification of variola, monkeypox, cowpox, and vaccinia viruses by multiplex real-time PCR assay. J Virol Methods. 2011;175:163–9. DOIPubMedGoogle Scholar
- Pfefferle S, Reucher S, Nörz D, Lütgehetmann M. Evaluation of a quantitative RT-PCR assay for the detection of the emerging coronavirus SARS-CoV-2 using a high throughput system. Euro Surveill. 2020;25:
2000152 . DOIPubMedGoogle Scholar - Müller G, Meyer A, Gras F, Emmerich P, Kolakowski T, Esposito JJ. Monkeypox virus in liver and spleen of child in Gabon. Lancet. 1988;1:769–70. DOIPubMedGoogle Scholar
- Poljak M, Korva M, Knap Gašper N, Fujs Komloš K, Sagadin M, Uršič T, et al. Clinical evaluation of the cobas SARS-CoV-2 test and a diagnostic platform switch during 48 hours in the midst of the COVID-19 pandemic. J Clin Microbiol. 2020;58:e00599–20. DOIPubMedGoogle Scholar
- Adler H, Gould S, Hine P, Snell LB, Wong W, Houlihan CF, et al. NHS England High Consequence Infectious Diseases (Airborne) Network. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022 May 24 [Epub ahead of print].
Figures
Tables
Cite This ArticleOriginal Publication Date: July 29, 2022
Table of Contents – Volume 28, Number 9—September 2022
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Marc Lütgehetmann, Institute of Medical Microbiology, Virology and Hygiene, Martinistraße 52, D-20246 Hamburg, Germany
Top